Corresponding author: Katsuhiro Yoshikawa, kyct1031@yahoo.co.jp
DOI: 10.31662/jmaj.2018-0038
Received: October 8, 2018
Accepted: January 18, 2018
Advance Publication: February 22, 2019
Published: March 4, 2019
Cite this article as:
Yoshikawa K, Miyata M, Sueoka N, Yamamoto D. Effective Steroid Therapy for Reexpansion Pulmonary Edema. JMA J. 2019;2(1):97-98.
Key words: Reexpansion pulmonary edema, Pleural effusion, Steroid pulse therapy, Chest drainage
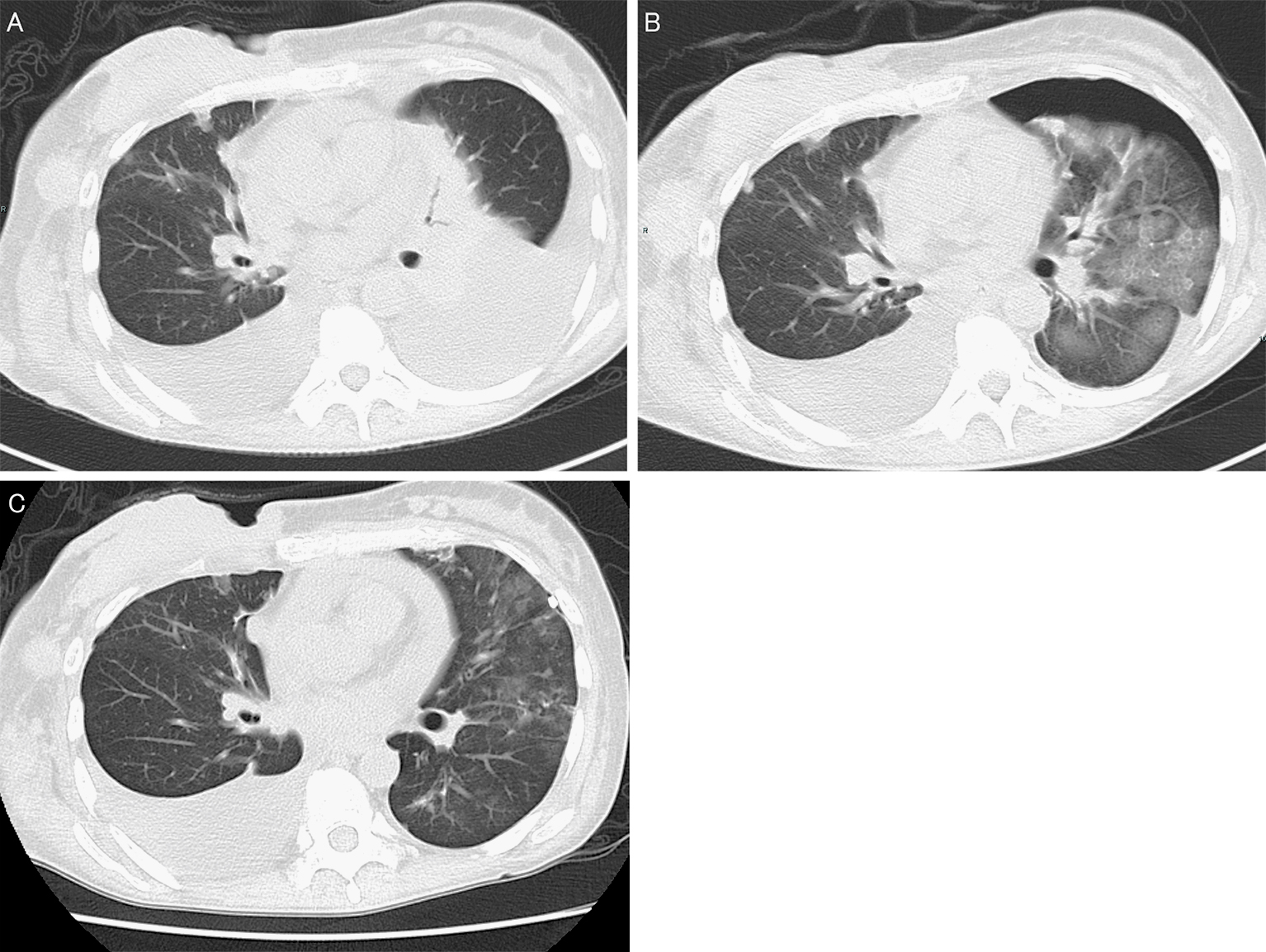
A 38-year-old woman was diagnosed with massive left pleural effusion caused by advanced breast cancer approximately 1 month ago (Figure 1A). A 12-French chest tube was placed, and 1000 mL of pleural effusion was drained for approximately 1 hour. No complications occurred. However, severe coughing and dyspnea developed upon completion of drainage. Coarse crackles were present in all left lung fields. Her peripheral blood oxygen saturation decreased to 93%. Computed tomography showed broad ground-glass opacities and poor expansion in the left lung, suggestive of reexpansion pulmonary edema (RPE) (Figure 1B). Methylprednisolone pulse therapy (1000 mg/day for 3 days) was administered. The symptoms improved the next day; after 4 days, computed tomography showed complete resolution of the radiological abnormalities (Figure 1C). RPE is rare (incidence, 0.2%) (1), but fatal (mortality rate, 20%) (2). Supportive therapy, such as positive pressure ventilation, is considered as the main treatment for RPE, but steroid pulse therapy also may be effective (3).
None
Katsuhiro Yoshikawa designed the study, and wrote the initial draft of the manuscript. All other authors have contributed to data collection and interpretation, and critically reviewed the manuscript. All authors approved the final version of the manuscript, and agree to be accountable for all aspects of the work with respect to ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
This study has been performed anonymously: therefore, approval by the IRB is not required based on Ethical Guidelines for Medical and Health Research Involving Human Subject by Ministry of Health, Labor and Welfare in Japan.
Written informed consent was obtained from the patient for publication of this “Image” and accompanying images.
Jones PW, Moyers JP, Rogers JT, et al. Ultrasound-guided thoracentesis: is it a safer method? Chest. 2003;123(2):418-23.
Mahfood S, Hix WR, Aaron BL, et al. Reexpansion pulmonary edema. Ann Thorac Surg. 1988;45(3):340-5.
Ozawa Y, Ichimura H, Sakai M. Reexpansion pulmonary edema after surgery for spontaneous pneumothorax in a patient with anorexia nervosa. Ann Med Surg. 2016;7:20-3.