Corresponding author: Kosei Takagi, kotakagi15@gmail.com
DOI: 10.31662/jmaj.2021-0062
Received: April 9, 2021
Accepted: June 16, 2021
Advance Publication: September 1, 2021
Published: October 15, 2021
Cite this article as:
Takagi K, Yagi T, Fujiwara T. Splenic and Peritoneal Metastases with Para-aortic and Virchow Lymph Node Metastases: Late Recurrence of Ovarian Cancer 30 Years after Initial Treatment. JMA J. 2021;4(4):428-431.
Key words: Ovarian cancer, late recurrence, splenic metastasis
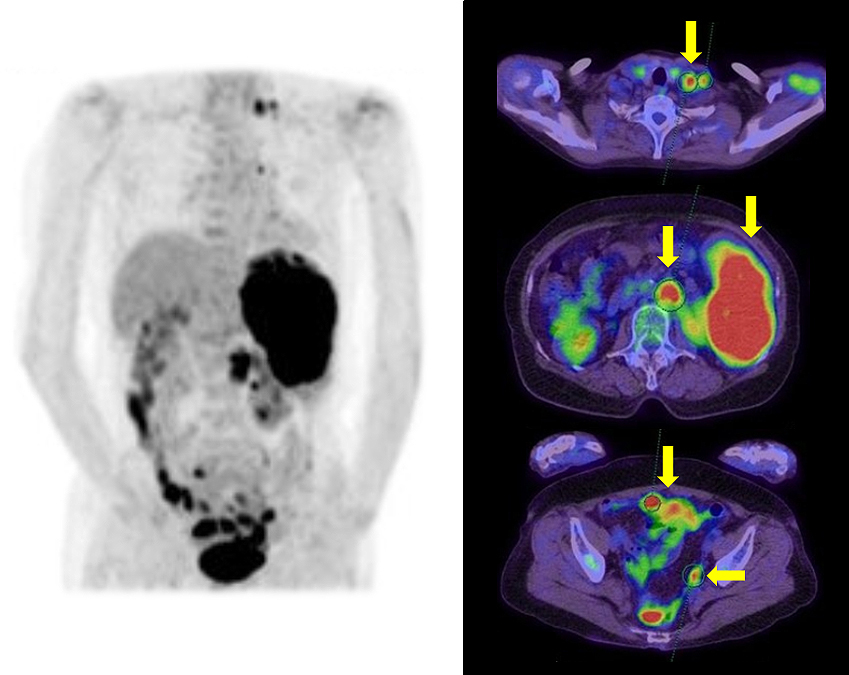
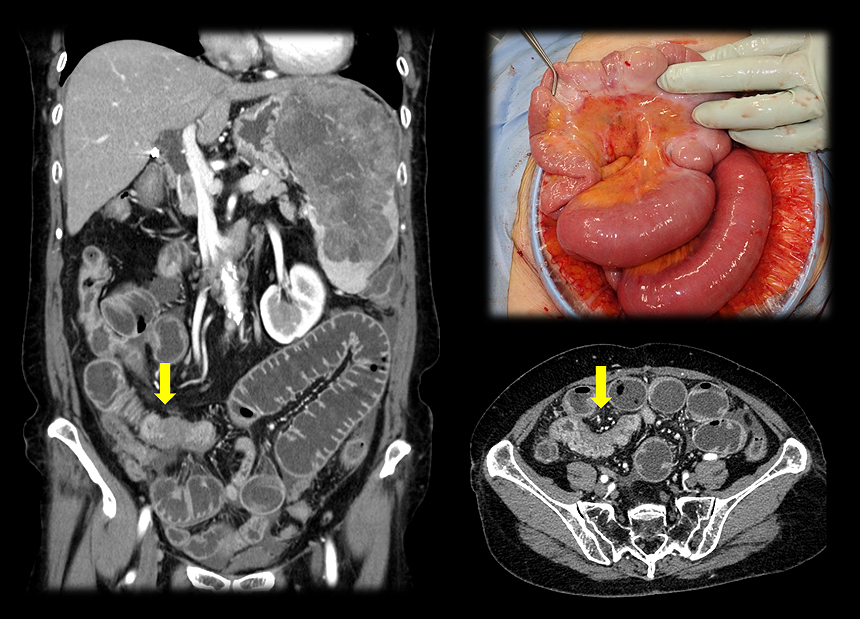
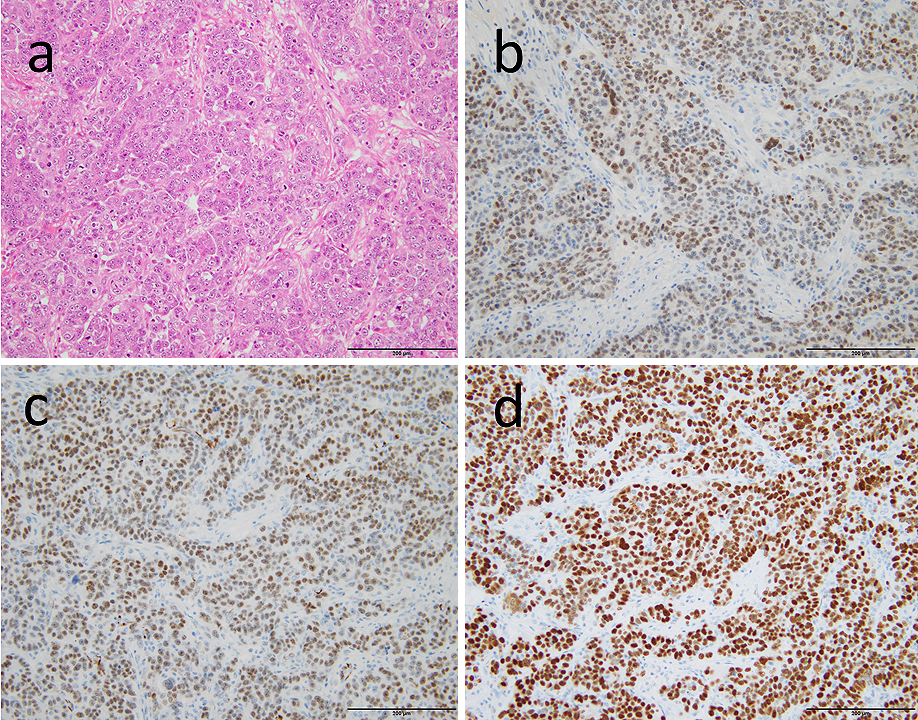
A 76-year-old woman presented with abdominal pain. The positron emission tomography (PET)/computed tomography (CT) revealed a large splenic tumor and peritoneal dissemination with para-aortic and Virchow lymphadenopathy, which were initially suspected of malignant lymphoma (Figure 1). Prior to further examination, the patient developed a mechanical bowel obstruction, requiring surgery with partial resection of the intestine (Figure 2). The patient had history of ovarian cancer treated with radical total hysterectomy and bilateral adnexectomy followed by adjuvant chemotherapy 30 years ago. Although no recurrence was observed during long-term follow-up, pathological findings of the resected intestine showed high-grade serous carcinoma (Figure 3). Immunohistochemically, the tumor cells were positive for PAX8, WT-1, and p53 and negative for TTF-1, CDX-2, mammaglobin, and GCDFP-15. Therefore, the patient was diagnosed with late recurrence of ovarian serous carcinoma. Thus far, only six cases with late recurrence, after 20 years, of ovarian cancer treated via surgery and chemotherapy have been reported (1), (2); however, this case is the first to demonstrate a recurrence of ovarian cancer more than 30 years after the initial treatment. Cancer stem cell might be associated with this recurrence (2), (3).
None
KT wrote the draft. All authors contributed equally to the manuscript. All authors edited, read, and approved the final manuscript.
Not applicable.
Written informed consent was obtained from the patient for publication of this report and any accompanying images.
Inoue E, Yotsumoto T, Inoue Y, et al. Mediastinal metastasis from ovarian serous carcinoma 29 years after initial treatment. Respir Med Case Rep. 2020;29:101003.
Menczer J, Schreiber L, Peled O, et al. Very late recurrence (after more than 20 years) of epithelial ovarian carcinoma: case report and literature review. Arch Gynecol Obstet. 2015;291(6):1199-203.
Lee H, Kwon OB, Lee JE, et al. Repositioning trimebutine maleate as a cancer treatment targeting ovarian cancer stem cells. Cells. 2021;10(4):918.