Corresponding author: Junya Tsurukiri, junya99@tokyo-med.ac.jp
DOI: 10.31662/jmaj.2024-0089
Received: May 2, 2024
Accepted: May 30, 2024
Advance Publication: October 8, 2024
Published: October 15, 2024
Cite this article as:
Izumi C, Tsurukiri J, Numata J, Nagura T, Sano H. Nonoperative Management for Traumatic Pseudoaneurysm of the Extrahepatic Portal Vein in an Older Adult. JMA J. 2024;7(4):630-632.
Key words: multiple trauma, hepatic injury, portal vein
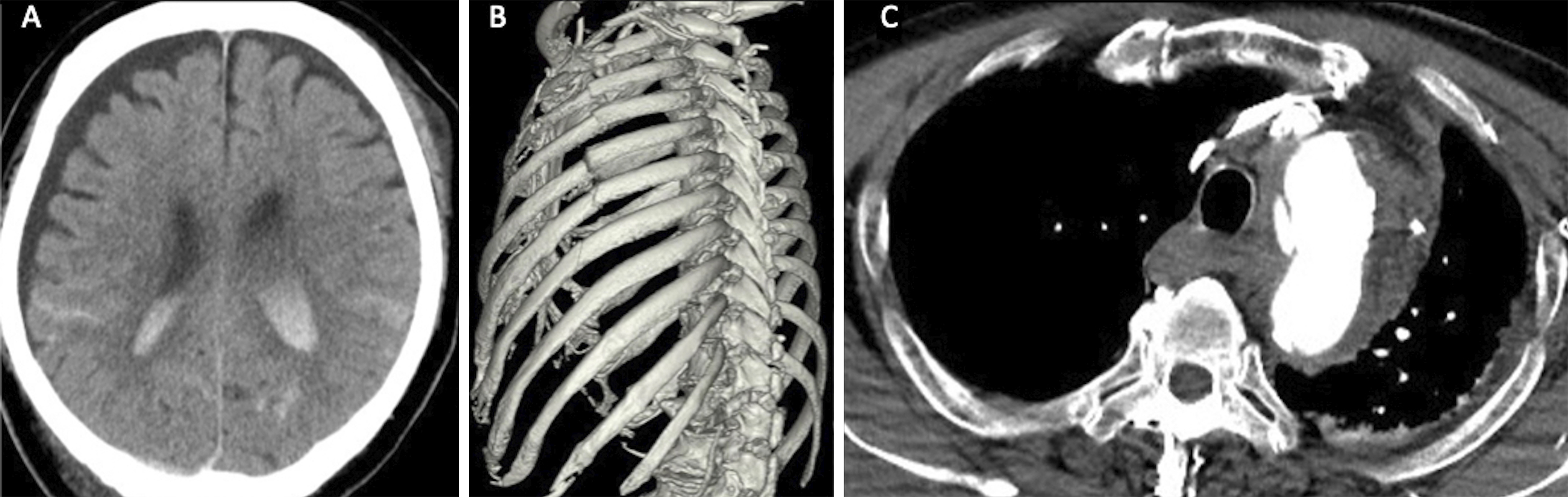
A 74-year-old man with hemorrhagic shock after a traffic accident was transferred to our emergency department. Contrast-enhanced computed tomography revealed intracranial and thoracic injuries (Figure 1), and the portal venous (PV) phase revealed a pseudoaneurysm of the superior mesenteric-PV (SMPV) confluence. Subsequently, the patient underwent nonoperative treatment with permissive hypotension. The traumatic PV pseudoaneurysm (tPVP) resolved three days posttreatment, and 20 days later, the diameter normalized (Figure 2).
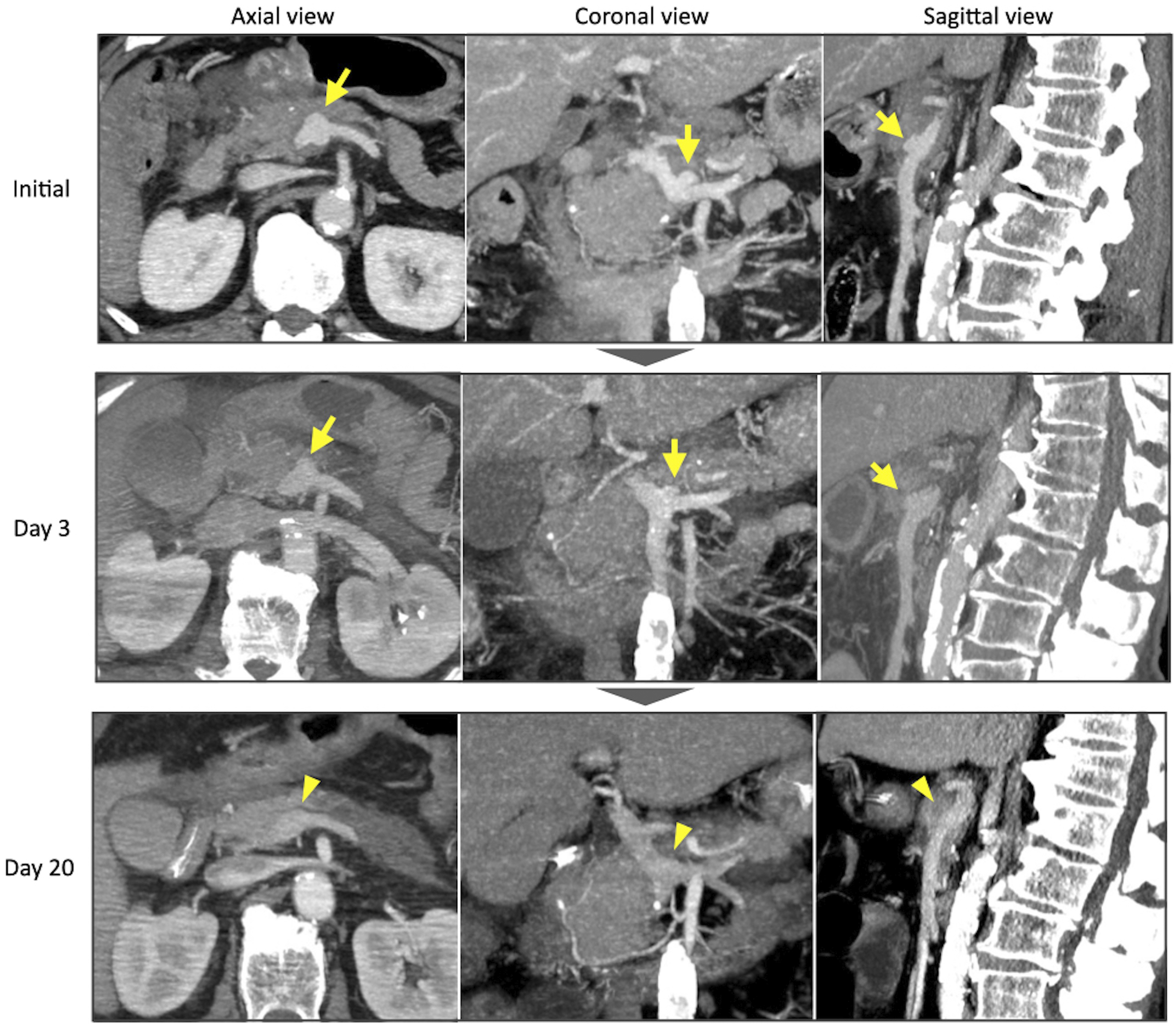
tPV injury is a rare (~0.1% of cases) and lethal complication frequently affecting the portal triad (1), (2). Most tPVPs are caused by the shear force of the mobile mesentery, leading to avulsion of the SMPV confluence (1). Furthermore, tPVP is difficult to diagnose clinically and is usually identified intraoperatively, with surgical venorrhaphy/ligation being the standard treatment, which poses a high mortality risk (3), (4). Our treatment results suggest that PV blood flow reduction with permissive hypotension and careful imaging followup may prevent tPVP rupture nonoperatively.
None
The authors would like to thank Enago (www.enago.jp) for the English language review.
Conceived and designed the experiments: IC, TJ
Contributed to interpretation of data: NJ, NT
Approved the final version to be submitted: TJ, SH
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Fraga GP, Bansal V, Fortlage D, et al. A 20-year experience with portal and superior mesenteric venous injuries: has anything changed? Eur J Vasc Endovasc Surg. 2009;37(1):87-91.
Pearl J, Chao A, Kennedy S, et al. Traumatic injuries to the portal vein: case study. J Trauma. 2004;56(4):779-82.
Hamanaka K, Hirokawa Y, Itoh T, et al. Successful non-operative management of traumatic extrahepatic portal venous injury without intraperitoneal hemorrhage: a case report. Acute Med Surg. 2016;4(2):205-8.
Buckman RF, Pathak AS, Badellino MM, et al. Portal vein injuries. Surg Clin North Am. 2001;81(6):1449-62.