Corresponding author: Yasuhito Hamaguchi, yasuhito@med.kanazawa-u.ac.jp
DOI: 10.31662/jmaj.2024-0154
Received: July 6, 2024
Accepted: August 5, 2024
Advance Publication: September 20, 2024
Published: October 15, 2024
Cite this article as:
Kimura A, Hamaguchi Y, Matsushita T. Dermatitis Herpetiformis Duhring. JMA J. 2024;7(4):635-637.
Key words: Dermatitis herpetiformis Duhring, IgA, diaminodiphenyl sulfone
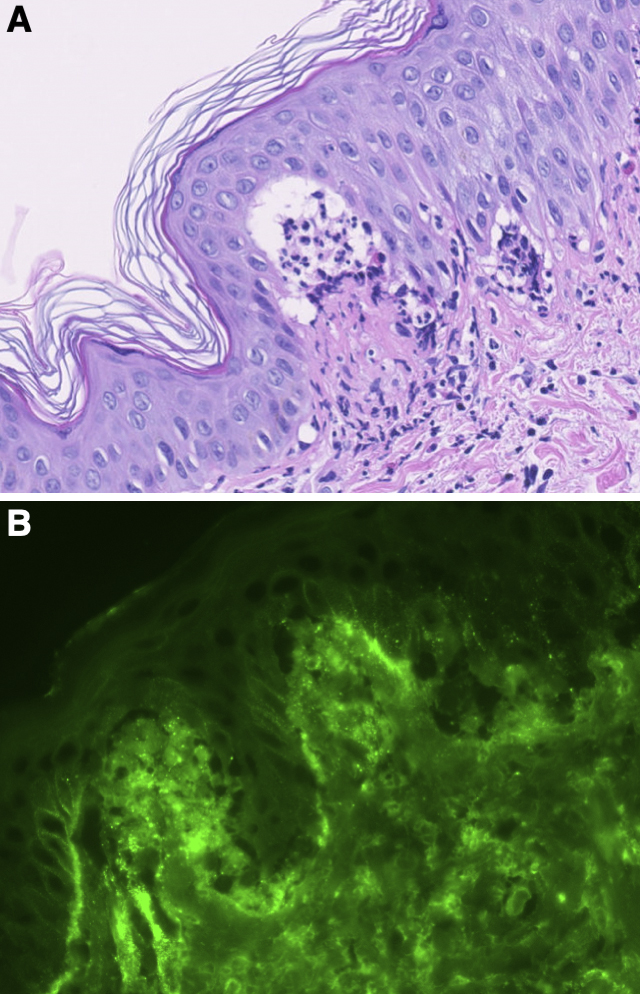
A 27-year-old Japanese man experienced severe pruritic erythema for 2 months. He had no symptoms of gluten-sensitive enteropathy. He was initially treated with topical corticosteroids, but his symptoms did not improve. On physical examination, erythematous plaques in an annular-to-continuous circle pattern were observed on the trunk and extremities (Figure 1A). Small vesicles accompanied some of these plaques. Skin biopsy is shown in Figure 2A. Direct immunofluorescence staining revealed IgA deposition in the dermal-epidermal junction papillae (Figure 2B). IgA anti-epidermal transglutaminase antibodies (106.7 AU/mL) and IgA anti-tissue glutaminase antibodies (35.8 AU/mL) were positive by ELISA (reference range, <22 AU/mL). A diagnosis of dermatitis herpetiformis Duhring was made. One month after the administration of diaminodiphenyl sulfone, the patient’s rash abated with pigmentation (Figure 1B). Clinical characteristics of dermatitis herpetiformis Duhring differ between Japanese and Caucasian individuals, with gluten sensitivity less common in Japan (1), (2).

None
The authors would like to thank Editage (www.editage.com) for the English language editing.
Drs. Matsushita and Hamaguchi had full access to all the data in this report and take responsibility for the integrity of the data and the accuracy of the data analysis.
Acquisition of data: Drs. Matsushita and Kimura.
Drafting of the manuscript: Drs. Matsushita, Hamaguchi, and Kimura.
Critical revision of the manuscript and approval of the final version to be submitted: Drs. Matsushita, Hamaguchi, and Kimura.
Written informed consent was obtained from the patient for the publication of this case report.
Ohata C, Ishii N, Niizeki H, et al. Unique characteristics in Japanese dermatitis herpetiformis. Br J Dermatol. 2016;174(1):180-3.
Barnadas MA. Dermatitis herpetiformis: a review of direct immunofluorescence findings. Am J Dermatopathol. 2016;38(4):283-8.