Corresponding author: Satoko Yamaguchi, syamaguc@m.u-tokyo.ac.jp
DOI: 10.31662/jmaj.2024-0337
Received: November 5, 2024
Accepted: April 28, 2025
Advance Publication: June 27, 2025
Introduction: Preventive programs, including cancer and diabetes screenings, were disrupted globally by the coronavirus disease 2019 (COVID-19) pandemic and had not returned to pre-pandemic levels even in 2021-2022. In Japan, COVID-19 was downgraded to the lowest-risk category under the Infectious Diseases Control Law in May 2023. However, whether participation in health check-ups recovered after this downgrade remains unclear. Additionally, understanding the impact of the pandemic on employees’ mental health and attrition is crucial for maintaining services in future pandemics. To address these issues, we conducted a nationwide survey.
Methods: A questionnaire survey was conducted between December 16, 2023, and February 21, 2024, targeting member facilities of Japan Society of Ningen Dock and Preventive Medical Care. The questionnaires covered COVID-19-related rules before and after the downgrade, the negative impact on employees’ mental health, and whether employee resignations increased compared to the pre-pandemic period. Participants also provided data on the number of health check-up examinees from 2019 to 2023.
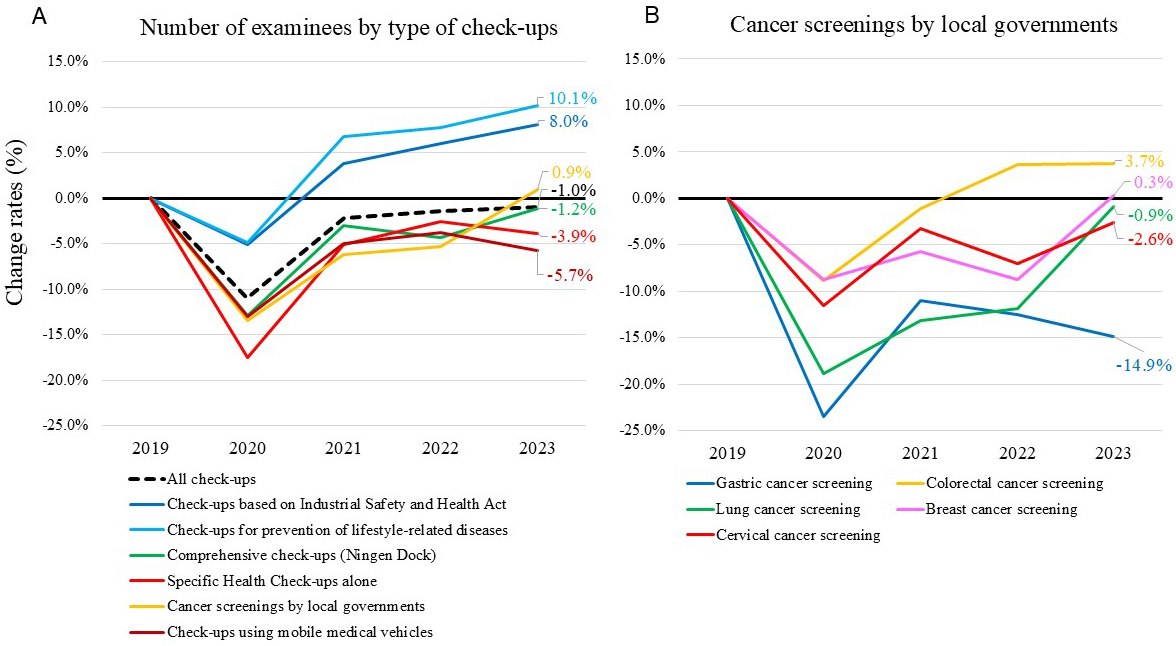
Results: We emailed 1,381 facilities, of which 856 responded (response rate: 62.0%). An additional 124 facilities responded via the Society’s website, yielding a total of 980 participants. While cancer screenings by local governments returned to pre-pandemic levels in 2023, gastric cancer screenings remained low. Nearly 30% of facilities reported a negative impact of the pandemic on employees’ mental health, which was associated with factors such as being annexed to hospitals and employees’ complaints about strict COVID-19-related rules. This negative impact was strongly linked to increased employee resignations.
Conclusions: While overall cancer screening rates recovered, gastric cancer screenings remained below pre-pandemic levels. Furthermore, the negative impact on employees’ mental health was significantly associated with increased attrition, highlighting the need for mental health support for those engaged in preventive medicine to maintain services during future pandemics.
Key words: COVID-19 pandemic, health check-up, cancer screening, mental health, attrition
In 2020, the coronavirus disease 2019 (COVID-19) pandemic caused significant worldwide disruptions to preventive programs, including cancer and diabetes screenings (1), (2), raising concerns regarding delayed diagnosis and treatment (3), (4). Reports suggested that cancer screenings remained below pre-pandemic levels even in 2021 (5), (6). Furthermore, it was reported that cervical cancer screening rates were lower in 2022 compared to the pre-pandemic level in the United States (7), and we also reported that the number of people undergoing non-mandatory cancer screenings had not recovered in 2022 (8).
Japan has developed nationwide health check-up programs. Employers are obliged to provide annual mandatory check-ups for full-time employees under the Industrial Safety and Health Act (9), and it is mandatory for employees to undergo them. All insurers are obliged to provide annual Specific Health Check-ups for all people aged 40-74 years (10). Additionally, local governments are required to make efforts to provide cancer screenings, but it is not mandatory for individuals to undergo them (11). We previously conducted two nationwide questionnaire surveys to investigate the impact of the pandemic on health check-ups, covering the periods from 2020 to 2021 and from 2020 to 2022 (8), (12). Although the number of examinees undergoing mandatory check-ups recovered in 2021 from the decline in 2020, the number of those undergoing non-mandatory check-ups remained low in 2021, and this tendency persisted into 2022. Moreover, employees in health check-up facilities were subject to strict COVID-19-related rules, leading to considerable sacrifices in their personal lives, a trend that was particularly evident in facilities annexed to hospitals.
In Japan, COVID-19 was downgraded on May 8, 2023, from the same category as novel influenza (equivalent to Category II) to a Category V infectious disease, the lowest-risk category under the Infectious Diseases Control Law, which is the same as that of seasonal influenza (13). Following the downgrade, non-pharmaceutical interventions (NPIs), such as screening and isolation of sick individuals, quarantine of exposed individuals, social distancing, and hand washing were lifted. Prior to this downgrade, mask-wearing guidelines were eased in March 2023; however, recommendations to wear masks in hospital or care home settings continued to protect those vulnerable to COVID-19 infection.
While evaluating the impact of the pandemic on examinees’ participation in health check-ups is important to prepare for future pandemics, the impact on employees working in health check-up facilities must also be considered. Preventing employee attrition is crucial to maintaining services, especially during crises such as pandemics and the subsequent recovery periods. Recent studies suggest that mental health has been a key factor contributing to attrition among healthcare workers since the COVID-19 pandemic (14), (15). Therefore, understanding the impact of the pandemic on employees’ mental health and the factors associated with this impact is crucial for sustaining healthcare services during future pandemics. Although the impact of the pandemic on healthcare workers, particularly regarding mental health and attrition, has been widely studied, its impact on those engaged in preventive programs remains unknown. A higher prevalence of mental health problems among healthcare workers was reported during the pandemic (16), (17), leading to increased workforce attrition. In Japan, some facilities are annexed to hospitals, with check-up facilities and hospitals typically located on the same premises. These facilities offer the advantage of immediate access to hospital resources if abnormalities are detected during health check-ups. Although employees of health check-up facilities are generally not working in high-risk units, which is a major risk factor for deteriorating mental health (16), (18), approximately half of the facilities annexed to hospitals reported that their employees had to contribute to COVID-19-related care in our previous survey (8). Moreover, COVID-19-related restrictions were reported to have adverse effects on mental health among the general population (19), (20), and employees of health check-up facilities were likely subject to more stringent COVID-19-related restrictions compared to others, even after the COVID-19 downgrade. Therefore, the mental health of employees in health check-up facilities was likely significantly impacted by the pandemic, even though they were not primarily involved in COVID-19-related care. In particular, facilities annexed to hospitals were more likely to provide COVID-19-related care and impose stricter COVID-19-related rules on their employees (8). These factors may have contributed to increased stress and a higher risk of mental health issues among employees.
This study, based on the third nationwide survey of healthcare facilities, examines the impact of the pandemic up to 2023, focusing on whether participation in health check-ups returned to pre-pandemic levels after NPIs were lifted. Additionally, it evaluates the pandemic’s effects on employees of health check-up facilities, particularly regarding mental health and attrition.
A questionnaire survey was administered, as previously described (8), (12). Briefly, healthcare facilities that were members of Japan Society of Ningen Dock and Preventive Medical Care and could respond via email were considered eligible. Japan Society of Ningen Dock and Preventive Medical Care had 1,813 member facilities at the time of the survey, including hospitals and clinics across Japan (21). Emails, including links to web-based questionnaires and fillable forms, were sent to eligible facilities on December 16, 2023. In addition, these links were made available on the Society’s homepage, so that member facilities that did not receive the emails could also respond.
The web-based questionnaires included questions on the type of facilities, the number of employees engaged in health check-ups per day, whether the facilities were providing inpatient or outpatient care for patients with COVID-19, precautions taken against COVID-19 to perform in-facility check-ups, and COVID-19-related rules in place during the year before and the period after the COVID-19 downgrade, whether the COVID-19 pandemic had a negative financial impact on the management of health check-ups, whether employee resignations increased or new recruits decreased compared to the pre-pandemic period, whether the pandemic had a negative impact on employees’ mental health, whether employees complained that COVID-19-related rules were too strict, and whether there were employees experiencing difficulty working due to post-COVID-19 condition, commonly known as long COVID. Facilities annexed to hospitals were asked about the number of beds and whether they provided emergency care. Additionally, to assess the degree of check-up facilities’ independence from annexed hospitals, facilities annexed to hospitals were asked whether personnel recruitment for check-up facilities was independent of recruitment for the annexed hospitals, and whether there was personnel transfer between the check-up facility and the annexed hospital.
Participants were also asked to fill in a form about the number of examinees who underwent health check-ups between 2019 and 2023, according to the type of check-ups. Responses were collected by February 21, 2024.
To evaluate whether the number of examinees undergoing health check-ups has returned to pre-pandemic levels, the total number of examinees undergoing check-ups in 2020, 2021, 2022, and 2023 was compared with that in 2019 (the pre-COVID-19 year) in 430 facilities that consistently provided data annually between 2019 and 2023. To evaluate the impact of the pandemic on employees’ mental health, facilities were asked whether it had a negative impact, and associated factors were identified as described below. Furthermore, the association between this negative impact and increased employee resignations was examined.
To assess the pandemic’s impact and the characteristics associated with its negative effect on employees’ mental health, facility characteristics were compared between hospital-annexed and non-annexed facilities and between facilities with and without the negative impact, using the χ2 test or Fisher’s exact test. To evaluate potential selection bias, facility characteristics were compared between participating and non-participating facilities using the χ2 test.
Precautions taken against COVID-19 to perform in-facility check-ups and COVID-19-related rules were compared before and after the COVID-19 downgrade using McNemar’s test.
To identify factors associated with the negative impact on employees’ mental health, multivariate logistic regression analyses were performed, with the negative impact on mental health as the dependent variable and facility characteristics, including type, scale, location, and COVID-19-related rules, as independent variables. The analyses were conducted after excluding one variable from each pair of variables with an absolute Spearman’s correlation coefficient greater than 0.6.
All statistical tests were two-sided, and P values < 0.05 were considered significant. All analyses were performed using R v4.2.3. (R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by the institutional review board of the Graduate School of Medicine at the University of Tokyo (2018030NI) and was performed in accordance with the relevant guidelines and regulations (the Declaration of Helsinki). The requirement for informed consent was waived because the facility-based survey did not contain any personal information.
Emails requesting participation in the survey were sent to 1,381 facilities, of which 856 responded (response rate 62.0%). In addition, 124 facilities that did not receive emails participated in the survey through the Japan Society of Ningen Dock and Preventive Medical Care website (Supplementary Figure 1). Overall, 980 facilities participated; 461 responded to both the web-based questionnaire and the fillable form, 498 responded to the web-based questionnaire only, and 21 responded to the fillable form only. To assess potential selection bias, the characteristics of facilities that participated in this study were compared with those that did not (Supplementary Table 1). The results suggested that facilities in the Hokkaido area may be underrepresented, while no differences were observed regarding urban location or public institution status.
We evaluated whether the number of examinees undergoing health check-ups has returned to the pre-pandemic levels in 2023. The total number of examinees undergoing check-ups at 430 facilities in each year between 2020 and 2023 was compared with that in 2019. As we previously reported, while the number of examinees undergoing “Check-ups based on Industrial Safety and Health Act” and “Check-ups for prevention of lifestyle-related diseases,” both primarily undertaken by full-time employees required to have annual health check-ups, recovered in 2021 from the decline in 2020, the number of examinees undergoing non-mandatory “Specific Health Check-ups alone” and “Cancer screenings by local governments” had not fully recovered even in 2022 (8). The change rates in the number of examinees undergoing non-mandatory “Specific Health Check-ups alone” and “Cancer screenings by local governments” in 2023 were −3.9% and 0.9%, respectively (Figure 1A and Supplementary Table 2). Among “Cancer screenings by local governments,” change rates for gastric, colorectal, lung, breast, and cervical cancer screenings were −14.9%, 3.7%, −0.9%, 0.3%, and −2.6%, respectively (Figure 1B).
We previously reported that the pandemic had a greater impact on health check-up facilities annexed to hospitals than on those not annexed. These facilities were more likely to provide COVID-19-related care, impose stricter COVID-19-related rules on their employees, and experience a negative financial impact (8). Therefore, we compared the characteristics between facilities annexed to hospitals and facilities not annexed to hospitals (Table 1). Among the 959 facilities that responded to the web-based questionnaire, 569 (59.3%) were annexed to hospitals, while 390 (40.7%) were not. Compared to facilities not annexed to hospitals, those annexed to hospitals were less likely to be in ordinance-designated cities or special wards in Tokyo, more likely to be public, have fewer employees, and provide inpatient and outpatient care for patients with COVID-19, consistent with the previous surveys (8), (12). Among the 569 facilities annexed to hospitals, personnel recruitment for check-up facilities was independent of recruitment for annexed hospitals in 243 (42.7%) facilities. Personnel transfers between check-up facilities and annexed hospitals occurred in 447 (78.6%) facilities, suggesting that the pandemic situation in the hospitals is relevant to employees in most check-up facilities annexed to hospitals.
Table 1. Characteristics of the Facilities That Participated in the Web-based Questionnaire by Facility Type.
| Total (n = 959) | Not annexed to hospitals (n = 390) | Annexed to hospitals (n = 569) | P valuea | ||
|---|---|---|---|---|---|
| Areab | Kanto | 331 (34.5) | 154 (39.5) | 177 (31.1) | 0.007 |
| Hokkaido | 19 (2.0) | 8 (2.1) | 11 (1.9) | ||
| Tohoku | 54 (5.6) | 23 (5.9) | 31 (5.4) | ||
| Chubu | 179 (18.7) | 60 (15.4) | 119 (20.9) | ||
| Kansai | 188 (19.6) | 87 (22.3) | 101 (17.8) | ||
| Chugoku | 73 (7.6) | 26 (6.7) | 47 (8.3) | ||
| Shikoku | 24 (2.5) | 9 (2.3) | 15 (2.6) | ||
| Kyushu | 82 (8.6) | 21 (5.4) | 61 (10.7) | ||
| Okinawa | 9 (0.9) | 2 (0.5) | 7 (1.2) | ||
| Location of facilities | Ordinance-designated cities/special wards in Tokyo | 379 (39.5) | 219 (56.2) | 160 (28.1) | <0.001 |
| Public or private institutions | Public | 182 (19.0) | 15 (3.8) | 167 (29.3) | <0.001 |
| Number of employees | 1-10 | 219 (22.8) | 73 (18.7) | 146 (25.7) | <0.001 |
| 11-20 | 249 (26.0) | 69 (17.7) | 180 (31.6) | ||
| 21-40 | 270 (28.2) | 92 (23.6) | 178 (31.3) | ||
| >40 | 221 (23.0) | 156 (40.0) | 65 (11.4) | ||
| Providing inpatient care for patients with COVID-19 | Yes | 482 (50.3) | 4 (1.0) | 478 (84.0) | <0.001 |
| Providing outpatient care for patients with COVID-19 | Yes | 648 (67.6) | 125 (32.1) | 523 (91.9) | <0.001 |
| Number of beds | <100 | N/A | N/A | 72 (12.7) | N/A |
| 100-299 | N/A | N/A | 282 (49.6) | ||
| 300-499 | N/A | N/A | 146 (25.7) | ||
| ≥500 | N/A | N/A | 63 (11.1) | ||
| Unanswered | N/A | N/A | 6 (1.1) | ||
| Emergency care | No emergency care | N/A | N/A | 71 (12.5) | N/A |
| Primary | N/A | N/A | 100 (17.6) | ||
| Secondary or tertiary | N/A | N/A | 391 (68.7) | ||
| Unanswered | N/A | N/A | 7 (1.2) | ||
| Personnel recruitment for check-up facilities is independent of recruitment for annexed hospitals | No | N/A | N/A | 321 (56.4) | N/A |
| Yes | N/A | N/A | 243 (42.7) | ||
| Unanswered | N/A | N/A | 5 (0.9) | ||
| Personnel transfer between the check-up facility and the annexed hospital | No | N/A | N/A | 118 (20.7) | N/A |
| Yes | N/A | N/A | 447 (78.6) | ||
| Unanswered | N/A | N/A | 4 (0.7) | ||
| Negative financial impact in 2023 | Yes | 235 (24.5) | 83 (21.3) | 152 (26.7) | 0.065 |
| Employee resignations compared to the pre-pandemic period | Increased | 104 (10.8) | 20 (5.1) | 84 (14.8) | <0.001 |
| New recruits in 2023 compared to 2019 | Decreased | 123 (12.8) | 29 (7.4) | 94 (16.5) | <0.001 |
| Employees complain that COVID-19-related rules are too strict | Yes | 73 (7.6) | 17 (4.4) | 56 (9.8) | 0.003 |
| Negative impact on the mental health of check-up facility employees | Yes | 280 (29.2) | 90 (23.1) | 190 (33.4) | <0.001 |
| Some employees have difficulty working due to long COVID | Yes | 74 (7.7) | 27 (6.9) | 47 (8.3) | 0.523 |
| Organizational social gathering involving meals held in FY2019/FY2023 | FY2019: no FY2023: no | 224 (23.4) | 96 (24.6) | 128 (22.5) | 0.069 |
| FY2019: no FY2023: yes | 227 (23.7) | 91 (23.3) | 136 (23.9) | ||
| FY2019: yes FY2023: no | 273 (28.5) | 95 (24.4) | 178 (31.3) | ||
| FY2019: yes FY2023: yes | 235 (24.5) | 108 (27.7) | 127 (22.3) | ||
| aP value comparing facilities annexed to hospitals and those not annexed using the χ2 test. bAreas of Japan: Japan comprises the four main islands of Hokkaido, Honshu, Shikoku, and Kyushu. Honshu, the largest island, is divided into Kanto (which includes the Greater Tokyo area), Tohoku, Chubu, Kansai, and Chugoku regions. Okinawa is the southernmost prefecture that includes the fifth-largest island. FY: fiscal year; N/A: not applicable. |
|||||
We evaluated whether the pandemic had a greater negative impact on facilities annexed to hospitals in terms of employees’ mental health and attrition. A negative impact on employees’ mental health was reported by 29.2% of all facilities, and indeed, facilities annexed to hospitals were more likely to report a negative impact on employees’ mental health compared to those not annexed to hospitals. Furthermore, facilities annexed to hospitals were more likely to report an increase in employee resignations and a decrease in new recruits compared to the pre-pandemic period. They were also more likely to report complaints from employees about COVID-19-related rules being too strict.
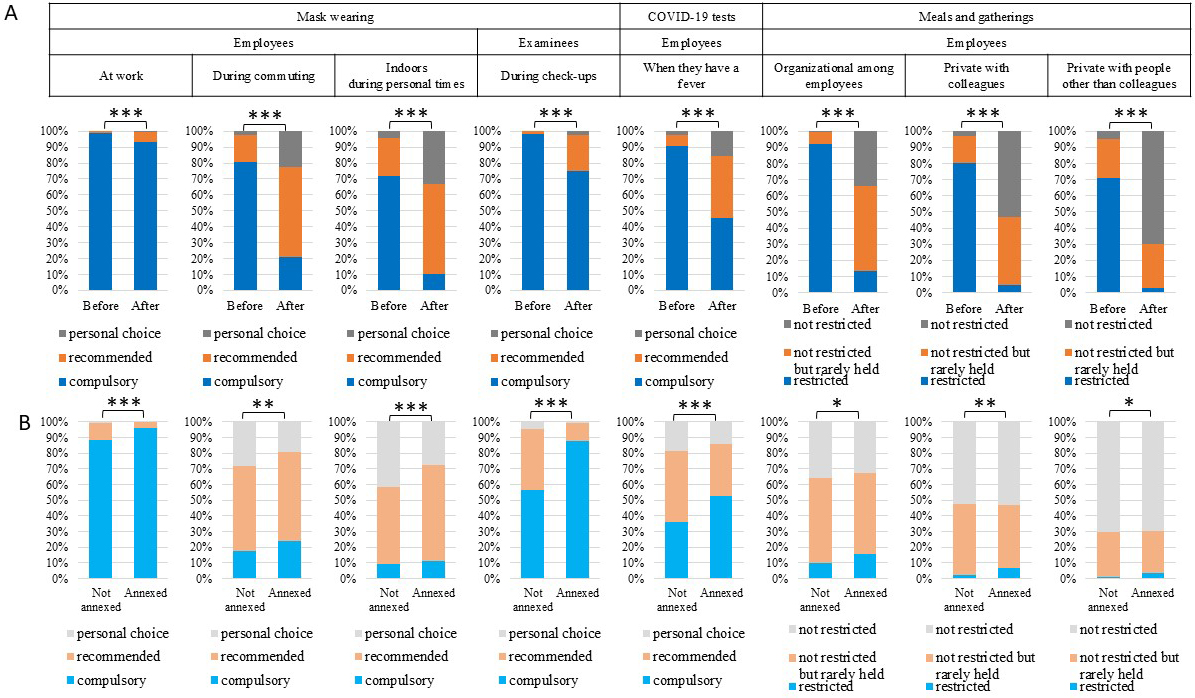
To evaluate the impact of the COVID-19 downgrade on precautions taken for in-facility check-ups and COVID-19-related rules, we compared the precautions and the COVID-19-related rules implemented during the year before and after the downgrade. We also evaluated whether employees in facilities annexed to hospitals were subject to stricter COVID-19-related rules than those in facilities not annexed to hospitals, even after the downgrade. The implementation rates of precautions declined (Supplementary Table 3 and Supplementary Figure 2), and COVID-19-related rules were generally relaxed after the COVID-19 downgrade (Table 2 and Figure 2); however, wearing masks at work was compulsory in more than 90% of the facilities even after the downgrade. Organizational social gatherings among employees involving meals and private meals and gatherings with people other than colleagues were restricted in over 90% and 70% of facilities, respectively, during the year before the downgrade. After the downgrade, restrictions were in place in 13.3% and 2.7% of facilities, respectively. However, 52.6% and 27.4% of the facilities reported that while such gatherings were not restricted, they were rarely held at the time of the survey. Facilities annexed to hospitals imposed stricter rules than those not annexed after the downgrade (Table 2 and Figure 2).
Table 2. COVID-19-related Rules before and after the Downgrade.
| Before vs after COVID-19 downgrade | After COVID-19 downgrade | ||||||
|---|---|---|---|---|---|---|---|
| Before (n = 959) | After (n = 959) | P valuea | Not annexed to hospitals (n = 390) | Annexed to hospitals (n = 569) | P valueb | ||
| Employees | |||||||
| Wearing masks at work | Compulsory | 951 (99.2) | 893 (93.1) | <0.001 | 345 (88.5) | 548 (96.3) | <0.001 |
| Recommended | 8 (0.8) | 62 (6.5) | 43 (11.0) | 19 (3.3) | |||
| Personal choice | 0 (0.0) | 4 (0.4) | 2 (0.5) | 2 (0.4) | |||
| Wearing masks during commuting | Compulsory | 771 (80.4) | 203 (21.2) | <0.001 | 68 (17.4) | 135 (23.7) | 0.002 |
| Recommended | 165 (17.2) | 538 (56.1) | 213 (54.6) | 325 (57.1) | |||
| Personal choice | 23 (2.4) | 218 (22.7) | 109 (27.9) | 109 (19.2) | |||
| Wearing masks indoors during personal time | Compulsory | 690 (71.9) | 101 (10.5) | <0.001 | 37 (9.5) | 64 (11.2) | <0.001 |
| Recommended | 230 (24.0) | 539 (56.2) | 191 (49.0) | 348 (61.2) | |||
| Personal choice | 39 (4.1) | 319 (33.3) | 162 (41.5) | 157 (27.6) | |||
| Taking COVID-19 tests when having a fever | Compulsory | 868 (90.5) | 438 (45.7) | <0.001 | 140 (35.9) | 298 (52.4) | <0.001 |
| Recommended | 68 (7.1) | 370 (38.6) | 178 (45.6) | 192 (33.7) | |||
| Personal choice | 23 (2.4) | 151 (15.7) | 72 (18.5) | 79 (13.9) | |||
| Number of days employees are not allowed to work after a COVID-19 infection | No restrictions | N/A | N/A | N/A | 12 (3.1) | 6 (1.1) | <0.001 |
| 5 days | N/A | N/A | 321 (82.3) | 396 (69.6) | |||
| 7 days | N/A | N/A | 48 (12.3) | 137 (24.1) | |||
| ≥10 days | N/A | N/A | 4 (1.0) | 22 (3.9) | |||
| Others | N/A | N/A | 5 (1.3) | 8 (1.4) | |||
| When family members are infected with COVID-19 | Employees are not allowed to work for a certain period | 901 (94.0) | 210 (21.9) | <0.001 | 70 (17.9) | 140 (24.6) | 0.045 |
| Employees are allowed to work if they are not sick | 57 (5.9) | 728 (75.9) | 310 (79.5) | 418 (73.5) | |||
| No restrictions | 1 (0.1) | 21 (2.2) | 10 (2.6) | 11 (1.9) | |||
| Organizational social gathering among employees involving meals (hospital-wide year-end party, department-wide farewell party) | Restricted | 884 (92.2) | 128 (13.3) | <0.001 | 38 (9.7) | 90 (15.8) | 0.024 |
| Not restricted but rarely held | 70 (7.3) | 504 (52.6) | 212 (54.4) | 292 (51.3) | |||
| Not restricted | 5 (0.5) | 327 (34.1) | 140 (35.9) | 187 (32.9) | |||
| Private meals and gatherings with colleagues | Restricted | 770 (80.3) | 48 (5.0) | <0.001 | 10 (2.6) | 38 (6.7) | 0.010 |
| Not restricted but rarely held | 163 (17.0) | 404 (42.1) | 176 (45.1) | 228 (40.1) | |||
| Not restricted | 26 (2.7) | 507 (52.9) | 204 (52.3) | 303 (53.3) | |||
| Private meals and gatherings with people other than colleagues | Restricted | 682 (71.1) | 26 (2.7) | <0.001 | 4 (1.0) | 22 (3.9) | 0.024 |
| Not restricted but rarely held | 228 (23.8) | 263 (27.4) | 113 (29.0) | 150 (26.4) | |||
| Not restricted | 49 (5.1) | 670 (69.9) | 273 (70.0) | 397 (69.8) | |||
| Examinees | |||||||
| Wearing masks When undergoing check-ups | Compulsory | 940 (98.0) | 719 (75.0) | <0.001 | 221 (56.7) | 498 (87.5) | <0.001 |
| Recommended | 18 (1.9) | 215 (22.4) | 150 (38.5) | 65 (11.4) | |||
| Personal choice | 1 (0.1) | 25 (2.6) | 19 (4.9) | 6 (1.1) | |||
| Undergoing check-ups after having a fever | Not allowed for a certain time | 842 (87.8) | 482 (50.3) | <0.001 | 157 (40.3) | 325 (57.1) | <0.001 |
| Allowed if the COVID-19 test is negative | 99 (10.3) | 216 (22.5) | 98 (25.1) | 118 (20.7) | |||
| Allowed if the fever has broken | 18 (1.9) | 261 (27.2) | 135 (34.6) | 126 (22.1) | |||
| The number of days examinees are not allowed to undergo check-ups after a COVID-19 infection | No restrictions | N/A | N/A | N/A | 48 (12.3) | 45 (7.9) | <0.001 |
| 5 days | N/A | N/A | 216 (55.4) | 191 (33.6) | |||
| 7 days | N/A | N/A | 59 (15.1) | 140 (24.6) | |||
| ≥10 days | N/A | N/A | 64 (16.4) | 188 (33.0) | |||
| Others | N/A | N/A | 3 (0.8) | 5 (0.9) | |||
| aP value comparing before and after the downgrade using McNemar’s test. bP value comparing facilities annexed to hospitals and those not annexed using the χ2 test. FY: fiscal year; N/A: not applicable. |
|||||||
Pulmonary function tests were suspended in most facilities during the pandemic (12), and we investigated whether the facilities restarted pulmonary function tests, because guidelines by the eight organizations related to health check-ups were updated based on recommendations for pulmonary function tests by the Japanese Respiratory Society after the COVID-19 downgrade (22). Facilities were asked when they restarted pulmonary function tests. The most frequent answer was that they were restarted in 2023 (52.8%), followed by responses that they were never interrupted (18.2%) and that they would be restarted in 2024 (11.7%) (Supplementary Figure 3).
Of the 959 facilities, 280 (29.2%) reported that the pandemic had a negative impact on the mental health of check-up facility employees (Table 1). We investigated factors associated with this negative impact. A negative impact on the mental health of employees was associated with being annexed to hospitals, providing inpatient and outpatient care for COVID-19, experiencing a negative financial impact in 2023, increased employee resignations, decreased new recruits in fiscal year (FY) 2023, employees complaining that COVID-19-related rules were too strict, and the presence of employees having difficulty working due to long COVID (Supplementary Table 4).
Multivariate analyses revealed that the negative impact on employees’ mental health was associated with being annexed to hospitals (odds ratio [OR] 1.69, 95% confidence interval [CI] 1.18-2.41), experiencing a negative financial impact in 2023 (OR 1.97, CI 1.42-2.75), employees complaining that COVID-19-related rules were too strict (OR 2.96, CI 1.77-4.96), and the presence of employees having difficulty working due to long COVID (OR 3.39, CI 2.03-5.66) (Table 3).
Table 3. Multivariate Logistic Regression Model for the Negative Impact on Mental Health of Employees.
| Univariate model | Multivariate model | ||||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | ||
| (Intercept) | - | - | 0.05 (0.02-0.14) | <0.001 | |
| Type of facility | Not annexed to hospitals | Ref | Ref | ||
| Annexed to hospitals | 1.67 (1.25-2.24) | <0.001 | 1.69 (1.18-2.41) | 0.004 | |
| Area | Kanto | Ref | Ref | ||
| Hokkaido | 0.78 (0.27-2.22) | 0.641 | 0.56 (0.17-1.85) | 0.344 | |
| Tohoku | 1.18 (0.65-2.17) | 0.582 | 1.11 (0.59-2.12) | 0.743 | |
| Chubu | 0.69 (0.46-1.04) | 0.079 | 0.64 (0.41-0.99) | 0.047 | |
| Kansai | 0.97 (0.66-1.43) | 0.893 | 1.03 (0.68-1.56) | 0.874 | |
| Chugoku | 0.66 (0.37-1.20) | 0.172 | 0.60 (0.32-1.12) | 0.106 | |
| Shikoku | 0.20 (0.05-0.86) | 0.031 | 0.23 (0.05-1.02) | 0.053 | |
| Kyushu | 1.01 (0.60-1.70) | 0.960 | 1.00 (0.58-1.74) | 0.995 | |
| Okinawa | 4.37 (1.07-17.8) | 0.040 | 3.02 (0.65-13.98) | 0.157 | |
| Location of facilities | Locations outside ordinance-designated cities or special wards in Tokyo | Ref | Ref | ||
| Ordinance-designated cities or special wards in Tokyo | 1.01 (0.76-1.34) | 0.960 | 1.03 (0.74-1.42) | 0.864 | |
| Public or private institutions | Private | Ref | Ref | ||
| Public | 1.10 (0.77-1.56) | 0.604 | 0.93 (0.63-1.38) | 0.720 | |
| Number of employees | 1-10 | Ref | Ref | ||
| 11-20 | 1.27 (0.85-1.89) | 0.250 | 0.45 (0.24-0.86) | 0.015 | |
| 21-40 | 1.28 (0.86-1.89) | 0.227 | 0.81 (0.45-1.46) | 0.490 | |
| >40 | 1.01 (0.66-1.54) | 0.960 | 0.64 (0.32-1.30) | 0.216 | |
| Negative financial impact in 2023 | Yes | 2.08 (1.53-2.83) | <0.001 | 1.97 (1.42-2.75) | <0.001 |
| Employees complain that COVID-19-related rules are too strict | Yes | 2.89 (1.78-4.68) | <0.001 | 2.96 (1.77-4.96) | <0.001 |
| Some employees have difficulty working due to long COVID | Yes | 3.57 (2.20-5.79) | <0.001 | 3.39 (2.03-5.66) | <0.001 |
| Wearing masks indoors during personal time | Personal choice | Ref | Ref | ||
| Compulsory or recommended | 1.36 (1.00-1.84) | 0.048 | 1.23 (0.86-1.76) | 0.250 | |
| Taking COVID-19 tests for fever | Personal choice | Ref | Ref | ||
| Compulsory or recommended | 0.93 (0.64-1.36) | 0.709 | 0.83 (0.54-1.27) | 0.384 | |
| When family members are infected with COVID-19 | No restriction/allowed to work if they are not sick | Ref | Ref | ||
| Employees are not allowed to work for a certain period | 1.05 (0.75-1.47) | 0.772 | 1.01 (0.70-1.46) | 0.963 | |
| Employees are recommended to receive the COVID-19 vaccination | Yes | 1.03 (0.78-1.36) | 0.833 | 0.84 (0.61-1.14) | 0.255 |
| Organizational social gathering among employees involving meals | Not restricted | Ref | Ref | ||
| Restricted/Not restricted but rarely held | 1.19 (0.88-1.60) | 0.263 | 1.28 (0.87-1.90) | 0.215 | |
| Private meals with people other than colleagues | Not restricted | Ref | Ref | ||
| Restricted/Not restricted but rarely held | 1.04 (0.77-1.41) | 0.802 | 0.81 (0.56-1.17) | 0.267 | |
| Organizational social gathering among employees involving meals held in FY2019/FY2023 | FY2019: no FY2023: no | Ref | Ref | ||
| FY2019: no FY2023: yes | 0.83 (0.55-1.24) | 0.360 | 0.95 (0.61-1.51) | 0.841 | |
| FY2019: yes FY2023: no | 0.88 (0.60-1.29) | 0.505 | 0.89 (0.59-1.34) | 0.571 | |
| FY2019: yes FY2023: yes | 0.86 (0.58-1.28) | 0.457 | 0.92 (0.58-1.45) | 0.715 | |
| FY: fiscal year; Ref: reference; CI: confidence interval. | |||||
Next, we assessed the impact of the pandemic on employee attrition and examined whether attrition was associated with the negative impact on employees’ mental health. Increased employee resignations compared to the pre-pandemic period were reported by 104 facilities (10.8%); while 5.1% of facilities not annexed to hospitals reported an increase, 14.8% of those annexed to hospitals did. Of the 104 facilities, 47 (45.2%), 46 (44.2%), 3 (2.9%) and 2 (1.9%) reported that resignations increased by <10%, 10%-30%, 30%-50%, and >50%, respectively (Figure 3 and Table 4). Among the job types with increased resignations, the highest frequency was observed among nurses (82.7%), followed by clerical workers (39.4%), clinical laboratory technologists (13.5%), doctors (11.5%), and other medical professionals (11.5%). The main reasons for this increase were increased workload due to patients with COVID-19 (68.3%), shortage of communications (35.6%), stress due to restrictions in private life (17.3%), and new jobs with better conditions (6.7%). Other reasons included an increased overall workload, a deterioration of working conditions due to the worsening financial situation, and a gap between actual work and expectations caused by a lack of pre-employment training.
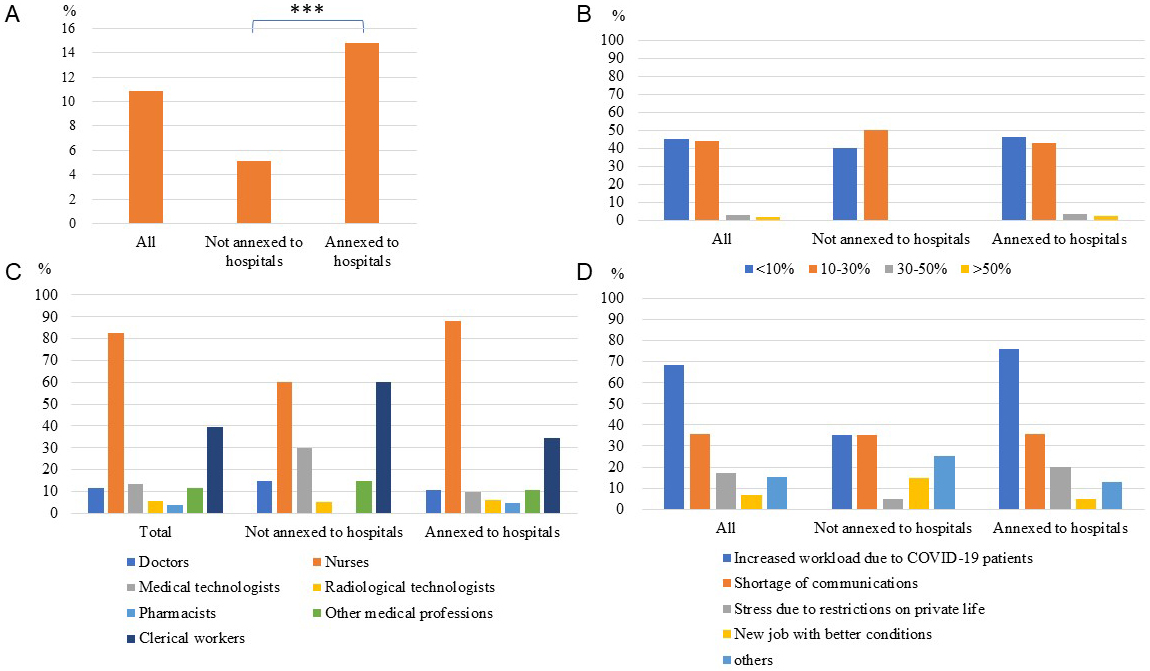
Table 4. Rate of Increase, Job Types, and the Reasons for Increased Employee Resignations.
| Total (n = 104) | Not annexed to hospitals (n = 20) | Annexed to hospitals (n = 84) | P value | ||
|---|---|---|---|---|---|
| Rate of increase in resignations compared to the pre-pandemic period (single answer) | <10% 10%-30% 30%-50% >50% |
47 (45.2) 46 (44.2) 3 (2.9) 2 (1.9) |
8 (40.0) 10 (50.0) 0 (0.0) 0 (0.0) |
39 (46.4) 36 (42.9) 3 (3.6) 2 (2.4) |
0.675 |
| Job types with increased resignations (multiple answers) | Doctors | 12 (11.5) | 3 (15.0) | 9 (10.7) | 0.881 |
| Nurses | 86 (82.7) | 12 (60.0) | 74 (88.1) | 0.008 | |
| Clinical laboratory technologists | 14 (13.5) | 6 (30.0) | 8 (9.5) | 0.041 | |
| Radiologic technologists | 6 (5.8) | 1 (5.0) | 5 (6.0) | >0.999 | |
| Pharmacists | 4 (3.8) | 0 (0.0) | 4 (4.8) | 0.728 | |
| Other medical professionals | 12 (11.5) | 3 (15.0) | 9 (10.7) | 0.881 | |
| Clerical workers | 41 (39.4) | 12 (60.0) | 29 (34.5) | 0.066 | |
| Reasons for increased resignation (multiple answers) | Increased workload due to patients with COVID-19 | 71 (68.3) | 7 (35.0) | 64 (76.2) | 0.001 |
| Shortage of communications | 37 (35.6) | 7 (35.0) | 30 (35.7) | >0.999 | |
| Stress due to restrictions in private life | 18 (17.3) | 1 (5.0) | 17 (20.2) | 0.197 | |
| New job with better conditions | 7 (6.7) | 3 (15.0) | 4 (4.8) | 0.252 | |
| Other reasons (below) | 16 (15.4) | 5 (25.0) | 11 (13.1) | 0.326 | |
| Other reasons (open-ended response) | Increased overall workload | 2 (1.9) | |||
| Deterioration of working conditions due to the worsening financial situation | 2 (1.9) | ||||
| A gap between the actual work and expectations due to the lack of pre-employment training | 2 (1.9) | ||||
| FY: fiscal year. | |||||
We evaluated the factors associated with an increase in employee resignations. An increase in employee resignations was associated with a negative impact on employees’ mental health, in addition to being annexed to hospitals, providing inpatient and outpatient care for patients with COVID-19, a negative financial impact in 2023, and a decrease in new recruits (Supplementary Table 5). Holding organizational social gatherings with meals (e.g., hospital-wide year-end parties, department-wide farewell parties) in FY2019 but not in FY2023 was associated with an increase in employee resignations. Conversely, not holding such gatherings in FY2019 but doing so in FY2023 was negatively associated with an increase in employee resignations.
An increase in employee resignations was strongly associated with a negative impact on the mental health of employees, even after multivariable adjustment (Table 5). Compared to not holding organizational social gatherings in either FY2019 or FY2023, holding one in FY2019 but not in FY2023 was marginally associated with an increase in employee resignations (P = 0.0503), while not holding one in FY2019 but in FY2023 was negatively associated.
Table 5. Multivariate Logistic Regression Model for Increased Resignation of Employees.
| Univariate model | Multivariate model | ||||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | ||
| (Intercept) | - | - | 0.05 (0.02-0.14) | <0.001 | |
| Type of facility | Not annexed to hospitals | Ref | Ref | ||
| Annexed to hospitals | 3.20 (1.93-5.31) | <0.001 | 2.83 (1.56-5.13) | <0.001 | |
| Area | Kanto | Ref | Ref | ||
| Hokkaido | 3.02 (1.03-8.89) | 0.045 | 2.85 (0.85-9.54) | 0.090 | |
| Tohoku | 1.06 (0.42-2.65) | 0.906 | 0.91 (0.34-2.43) | 0.852 | |
| Chubu | 1.12 (0.63-2.00) | 0.690 | 0.99 (0.53-1.86) | 0.977 | |
| Kansai | 0.84 (0.46-1.55) | 0.577 | 0.84 (0.44-1.62) | 0.611 | |
| Chugoku | 0.90 (0.38-2.11) | 0.803 | 0.92 (0.37-2.31) | 0.862 | |
| Shikoku | 0.37 (0.05-2.81) | 0.335 | 0.51 (0.06-4.12) | 0.529 | |
| Kyushu | 1.04 (0.48-2.27) | 0.916 | 0.95 (0.41-2.20) | 0.913 | |
| Okinawa | 4.23 (1.01-17.66) | 0.048 | 2.39 (0.42-13.44) | 0.324 | |
| Location of facilities | Locations outside ordinance-designated cities or special wards in Tokyo | Ref | Ref | ||
| Ordinance-designated cities or special wards in Tokyo vs others | 0.95 (0.63-1.45) | 0.815 | 1.25 (0.77-2.02) | 0.376 | |
| Public or private institutions | Private | Ref | Ref | ||
| Public | 1.58 (0.99-2.54) | 0.056 | 1.13 (0.66-1.92) | 0.660 | |
| Number of employees | 1-10 | Ref | Ref | ||
| 11-20 | 0.60 (0.33-1.09) | 0.095 | 0.45 (0.24-0.86) | 0.015 | |
| 21-40 | 1.01 (0.60-1.70) | 0.976 | 0.81 (0.45-1.46) | 0.490 | |
| >40 | 0.58 (0.31-1.08) | 0.086 | 0.64 (0.32-1.30) | 0.216 | |
| Negative financial impact in 2023 | Yes | 1.75 (1.13-2.69) | 0.012 | 1.35 (0.84-2.18) | 0.213 |
| Employees complain that COVID-19 related rules are too strict | Yes | 1.89 (1.00-3.58) | 0.0498 | 1.20 (0.59-2.45) | 0.615 |
| Some employees have difficulty in working due to long COVID | Yes | 1.31 (0.65-2.65) | 0.443 | 0.79 (0.35-1.75) | 0.558 |
| Wearing masks indoors in private time | Personal choice | Ref | Ref | ||
| Compulsory or recommended | 1.03 (0.67-1.59) | 0.896 | 0.76 (0.45-1.26) | 0.285 | |
| Taking COVID-19 tests for fever | Personal choice | Ref | Ref | ||
| Compulsory or recommended | 0.95 (0.55-1.65) | 0.859 | 0.87 (0.46-1.64) | 0.660 | |
| When family members are infected with COVID-19 | No restriction/allowed to work if they are not sick | Ref | Ref | ||
| Employees are not allowed to work for a certain period | 0.95 (0.58-1.57) | 0.846 | 0.83 (0.48-1.44) | 0.505 | |
| Employees are recommended to receive the COVID-19 vaccination | Yes | 1.54 (1.02-2.33) | 0.040 | 1.41 (0.88-2.24) | 0.150 |
| Organizational social gathering among employees involving meals | Not restricted | Ref | Ref | ||
| Restricted or rarely held | 1.31 (0.84-2.05) | 0.232 | 1.01 (0.55-1.85) | 0.972 | |
| Private meals with people other than colleagues | Not restricted | Ref | Ref | ||
| Restricted or rarely held | 0.98 (0.63-1.53) | 0.938 | 0.94 (0.55-1.60) | 0.814 | |
| Organizational social gathering among employees involving meals held in FY2019/FY2023 | FY2019: no FY2023: no | Ref | Ref | ||
| FY2019: no FY2023: yes | 0.38 (0.17-0.84) | 0.017 | 0.35 (0.15-0.83) | 0.017 | |
| FY2019: yes FY2023: no | 1.81 (1.05-3.12) | 0.032 | 1.79 (1.00-3.21) | 0.0503 | |
| FY2019: yes FY2023: yes | 1.24 (0.69-2.24) | 0.472 | 1.14 (0.58-2.25) | 0.703 | |
| Negative impact on the mental health of employees | Yes | 3.44 (2.27-5.21) | <0.001 | 3.26 (2.07-5.15) | <0.001 |
| FY: fiscal year; Ref: reference; CI: confidence interval. | |||||
We previously reported that approximately 60% of the facilities reported a negative financial impact on the management of health check-ups, even in 2022 (8). Therefore, we assessed the extent of this impact in 2023. A negative financial impact on the management of check-up facilities in 2023 was reported by 235 (24.5%) facilities, with no significant difference between hospital-annexed and non-annexed facilities (Table 1). The most frequent reason for the negative financial impact was that examinees who avoided visits during the COVID-19 pandemic had not returned (60.4%), followed by increased costs due to precautions against COVID-19 (51.5%), limiting appointments due to staff shortages (24.7%) and other reasons (17.0%), including last-minute cancellations due to sickness (5.5%) and limiting appointments as a precaution against COVID-19 (4.3%) (Supplementary Table 6).
In this nationwide follow-up survey of healthcare facilities, conducted after the COVID-19 downgrade in 2023, we report that the number of examinees undergoing non-mandatory cancer screenings provided by local governments finally recovered to the pre-pandemic level in 2023 (Figure 1). However, gastric cancer screenings remained below pre-pandemic levels, raising concerns about delayed diagnoses. Additionally, nearly 30% of the facilities reported a negative impact on employees’ mental health, with factors such as being annexed to hospitals and employees’ complaints about strict COVID-19-related rules associated with this negative impact. Notably, increased employee resignations were also linked to this negative mental health impact.
Cancer screening programs were disrupted during the early phase of the pandemic globally (23), (24), (25). More recent studies revealed that cancer screenings had not fully recovered to the pre-pandemic levels even in 2022 (7), (8), (26). In our previous surveys, we found that while the number of examinees undergoing mandatory check-ups recovered by 2021 from the decline during the COVID-19 pandemic, the number of those undergoing non-mandatory check-ups remained low in 2021 (12), a tendency that persisted into 2022 (8). The result that it has taken three years for these screenings to recover to the pre-pandemic levels, raises concerns about delays in diagnosis and highlights a challenge for future pandemics. It remains to be determined which characteristics of the examinees were most impacted by the pandemic. Healthcare policies should specifically target these individuals during future pandemics to improve screening rates. Targeted outreach programs emphasizing the importance of timely screenings could help improve participation rates and minimize delays in diagnosis.
A negative impact on employees’ mental health due to the COVID-19 pandemic was reported by 29.2% of the facilities; 23.1% of those not annexed to hospitals and 33.4% of those annexed to hospitals reported this negative impact. The pandemic imposed unprecedented stress on healthcare professionals, and a wide range of mental health problems among healthcare workers, such as depression, anxiety, post-traumatic stress, and insomnia, have been reported (16), (17). Reported risk factors included being female, working in high-risk units, and providing direct care for patients with COVID-19 (16), though non-frontline healthcare workers were also experiencing psychological distress (27). Although our study focused on health check-up facilities, where employees are generally not in high-risk settings, our findings suggest that many of these staff members were nevertheless impacted by the hospital pandemic environment. Approximately 60% of the participating facilities were annexed to hospitals, and of these, over 80% provided both inpatient and outpatient care for patients with COVID-19. Importantly, nearly 80% of annexed facilities reported personnel transfers between the check-up facility and the hospital. Furthermore, our previous survey indicated that approximately half of the annexed facilities required health check-up staff to assist with COVID-19-related care (8). These results suggest that, during the pandemic, personnel working in health check-up facilities were often involved in clinical duties or subjected to hospital-level infection control measures, which may have contributed to their mental health burden. The negative impact on employees’ mental health was associated with being annexed to hospitals, experiencing a negative financial impact in 2023, employees complaining that COVID-19-related rules were too strict, and the presence of employees having difficulty working due to long COVID (Table 3). Although we did not find significant associations with specific COVID-19-related rules, such as wearing masks, taking COVID-19 tests, or holding meals and gatherings, previous reports have suggested that COVID-19-related restrictions were associated with mental health problems (19). As healthcare workers were subject to stricter restrictions for a longer period than others, it is possible that these restrictions contributed to the negative impact on their mental health. Indeed, our results revealed that employees in facilities annexed to hospitals were subject to stricter COVID-19-related restrictions in almost every aspect compared to those in facilities not annexed to hospitals, even after the downgrade. Long COVID has also been reported to affect mental health (28).
Understanding the factors influencing attrition and taking measures to prevent it is crucial, especially during healthcare crises such as pandemics, to ensure the continuity of healthcare services. Mental health is a key factor, but other factors such as increased workload, financial pressures, and workplace relationships also contribute to attrition. A recent study analyzing factors associated with the attrition of UK healthcare workers since the COVID-19 pandemic reported a strong association between the desire to leave healthcare and mental health measures (15). This highlights the need to integrate mental health support to mitigate attrition. Adverse mental health can lead to increased attrition among healthcare workers (17), and reports have suggested that the intention to leave one’s job among healthcare professionals was high during the pandemic (29), (30), (31), (32). Consistent with previous reports, the negative impact on employees’ mental health was strongly associated with increased resignations in this study. In addition, holding organizational social gatherings involving meals in FY2019 but not in FY2023 was marginally associated with increased resignations, while not holding such gatherings in FY2019 but doing so in FY2023 was negatively associated with increased resignations. This suggests that more active communication among co-workers might have helped prevent employee resignations. The highest frequency of increased resignations was observed among nurses, and the most common reason for increased resignations was the increased workload due to patients with COVID-19. Providing mental health support and fostering active communication among employees may be crucial for preventing attrition during future pandemics.
The key strength of this study is that it was a large-scale nationwide survey conducted in Japan, achieving a response rate of over 60%. We uncovered the impact of the COVID-19 pandemic on health check-ups up to 2023, covering the periods before and after the COVID-19 downgrade. Moreover, we compared the precautions against COVID-19 and COVID-19-related rules during the year before and the period after the COVID-19 downgrade. To the best of our knowledge, this is the first large-scale study to investigate the negative impact on the mental health of check-up facility employees due to the COVID-19 pandemic.
This study had several limitations. First, the survey was completed by a representative from each facility; therefore, the negative impact on employees’ mental health may have been influenced by their personal impressions. Second, due to the unique nature of Japan’s health check-up system, these results may not be applicable to other regions. Third, there may be selection bias in the participating facilities, as the exact total number of facilities providing health check-ups, including non-members of Japan Society of Ningen Dock and Preventive Medical Care, is unavailable.
Although the number of examinees participating in non-mandatory cancer screenings provided by local governments returned to pre-pandemic levels in 2023, the number for gastric cancer screenings remained low. An increase in employee resignations in check-up facilities was associated with a negative impact on the mental health of employees, which in turn was linked to being annexed to hospitals, experiencing a negative financial impact in 2023, employees complaining that COVID-19-related rules were too strict, and the presence of employees having difficulty working due to long COVID. Providing mental health support to healthcare workers, including those engaged in preventive medicine, is especially important during pandemics to prevent attrition and maintain healthcare services.
Satoko Yamaguchi, Akira Okada, Reiko Inoue, and Takashi Kadowaki are members of the Department of Prevention of Diabetes and Lifestyle-related Diseases, which is a cooperative program between the University of Tokyo and Asahi Mutual Life Insurance Company. Tomofumi Atarashi, Shigeru Nasu, Toshimasa Yamauchi, Yasuji Arase, Takao Aizawa, and Masaomi Nangaku declare no competing interests.
This work was supported by MHLW Research on Emerging and Re-emerging Infectious Diseases and Immunization (Program Grant Numbers JPMH23HA2011 and JPMH24HA2015). The funding organization has no role in the design of the study, analysis, interpretation of data, or writing the manuscript.
We would like to thank all the participating facilities for taking the time to respond to the questionnaire. We thank Ms. Emi Yoshikawa and Mr. Shoji Negishi of Japan Society of Ningen Dock and Preventive Medical Care for their assistance in this study.
Satoko Yamaguchi, Tomofumi Atarashi, Akira Okada, Shigeru Nasu, Masaomi Nangaku, and Takashi Kadowaki designed the study. Tomofumi Atarashi and Shigeru Nasu acquired data. Satoko Yamaguchi analyzed the data. Satoko Yamaguchi and Takashi Kadowaki wrote the first draft of the manuscript. All authors contributed to the interpretation of data and reviewed, revised, and approved the final manuscript. Satoko Yamaguchi and Tomofumi Atarashi contributed equally as first authors.
This study was approved by the institutional review board of the Graduate School of Medicine at the University of Tokyo (2018030NI) and was performed in accordance with the relevant guidelines and regulations (the Declaration of Helsinki). The requirement for informed consent was waived because the facility-based survey did not contain any personal information.
Teglia F, Angelini M, Astolfi L, et al. Global association of COVID-19 pandemic measures with cancer screening: a systematic review and meta-analysis. JAMA Oncol. 2022;8(9):1287-93.
Carr MJ, Wright AK, Leelarathna L, et al. Impact of COVID-19 on diagnoses, monitoring, and mortality in people with type 2 diabetes in the UK. Lancet Diabetes Endocrinol. 2021;9(7):413-15.
Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023-34.
de Jonge L, Worthington J, van Wifferen F, et al. Impact of the COVID-19 pandemic on faecal immunochemical test-based colorectal cancer screening programmes in Australia, Canada, and the Netherlands: a comparative modelling study. Lancet Gastroenterol Hepatol. 2021;6(4):304-14.
Oakes AH, Boyce K, Patton C, et al. Rates of routine cancer screening and diagnosis before vs after the COVID-19 pandemic. JAMA Oncol. 2023;9(1):145-46.
Machii R, Takahashi H, Miyazawa J, et al. Cancer screening in Japan 2 years after the COVID-19 pandemic: changes in participation, 2017-2021. Prev Med Rep. 2024;39:102649.
Borders TF, Thaxton Wiggins A. Cervical cancer screening rates among rural and urban females, from 2019 to 2022. JAMA Netw Open. 2024;7(6):e2417094.
Yamaguchi S, Atarashi T, Okada A, et al. Impact of the COVID-19 pandemic on health check-ups in 2021 and 2022: a nationwide follow-up survey of healthcare facilities in Japan Society of Ningen Dock. JMA J. 2024;7(1):94-105.
OECD reviews of public health: Japan [Internet]. Organisation for Economic Co-operation and Development [cited 2024 Oct 22]. Available from: https://www.oecd-ilibrary.org/sites/9789264311602-7-en/index.html?itemId=/content/component/9789264311602-7-en
Tsushita K, Hosler AS, Miura K, et al. Rationale and descriptive analysis of specific health guidance: the nationwide lifestyle intervention program targeting metabolic syndrome in Japan. J Atheroscler Thromb. 2018;25(4):308-22.
Cancer screenings [Internet]. Ministry of Health, Labour and Welfare [cited 2024 Oct 22]. Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000059490.html
Yamaguchi S, Atarashi T, Okada A, et al. Impact of the COVID-19 pandemic on health check-ups: a nationwide questionnaire survey in 639 healthcare facilities in Japan Society of Ningen Dock. JMA J. 2023;6(3):321-31.
Kitahara K, Nishikawa Y, Yokoyama H, et al. An overview of the reclassification of COVID-19 of the Infectious Diseases Control Law in Japan. Glob Health Med. 2023;5(2):70-4.
DePierro JM, Chan CC, Mohamed N, et al. Determinants of staff intent to leave health care during the COVID-19 pandemic. Am J Public Health. 2024;114(suppl 2):200-3.
Martin CA, Medisauskaite A, Guyatt AL, et al. Factors associated with attrition from the UK healthcare workforce since the COVID-19 pandemic: results from a nationwide survey study. Lancet Reg Health Eur. 2024;47:101133.
Lee BEC, Ling M, Boyd L, et al. The prevalence of probable mental health disorders among hospital healthcare workers during COVID-19: a systematic review and meta-analysis. J Affect Disord. 2023;330:329-45.
Collett G, Korszun A, Gupta AK. Potential strategies for supporting mental health and mitigating the risk of burnout among healthcare professionals: insights from the COVID-19 pandemic. eClinicalMedicine. 2024;71:102562.
De Brier N, Stroobants S, Vandekerckhove P, et al. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): a rapid systematic review. PLoS One. 2020;15(12):e0244052.
Witteveen AB, Young SY, Cuijpers P, et al. COVID-19 and common mental health symptoms in the early phase of the pandemic: an umbrella review of the evidence. PLoS Med. 2023;20(4):e1004206.
Sojli E, Tham WW, Bryant R, et al. COVID-19 restrictions and age-specific mental health-U.S. probability-based panel evidence. Transl Psychiatry. 2021;11(1):418.
Lu J. Ningen Dock: Japan’s unique comprehensive health checkup system for early detection of disease. Glob Health Med. 2022;4(1):9-13.
Pulmonary function tests in the time of COVID-19 [Internet]. The Japanese Respiratory Society [cited 2024 Oct 22]. Available from: https://www.jrs.or.jp/information/jrs/20230517144955.html
Chen RC, Haynes K, Du S, et al. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021;7(6):878-84.
Peacock HM, Tambuyzer T, Verdoodt F, et al. Decline and incomplete recovery in cancer diagnoses during the COVID-19 pandemic in Belgium: a year-long, population-level analysis. ESMO Open. 2021;6(4):100197.
Walker MJ, Meggetto O, Gao J, et al. Measuring the impact of the COVID-19 pandemic on organized cancer screening and diagnostic follow-up care in Ontario, Canada: a provincial, population-based study. Prev Med. 2021;151:106586.
Doan C, Li S, Goodwin JS. Breast and lung cancer screening among medicare enrollees during the COVID-19 pandemic. JAMA Netw Open. 2023;6(2):e2255589.
Norhayati MN, Che Yusof R, Azman MY. Depressive symptoms among frontline and non-frontline healthcare providers in response to the COVID-19 pandemic in Kelantan, Malaysia: a cross sectional study. PLoS One. 2021;16(8):e0256932.
Hawke LD, Nguyen ATP, Ski CF, et al. Interventions for mental health, cognition, and psychological wellbeing in long COVID: a systematic review of registered trials. Psychol Med. 2022;52(13):2426-40.
Sinsky CA, Brown RL, Stillman MJ, et al. COVID-related stress and work intentions in a sample of US health care workers. Mayo Clin Proc Innov Qual Outcomes. 2021;5(6):1165-73.
Tolksdorf KH, Tischler U, Heinrichs K. Correlates of turnover intention among nursing staff in the COVID-19 pandemic: a systematic review. BMC Nurs. 2022;21(1):174.
Poon YR, Lin YP, Griffiths P, et al. A global overview of healthcare workers’ turnover intention amid COVID-19 pandemic: a systematic review with future directions. Hum Resour Health. 2022;20(1):70.
Nigam JAS, Barker RM, Cunningham TR, et al. Vital Signs: Health Worker-Perceived Working Conditions and Symptoms of Poor Mental Health - Quality of Worklife Survey, United States, 2018-2022. MMWR Morb Mortal Wkly Rep. 2023;72(44):1197-205.