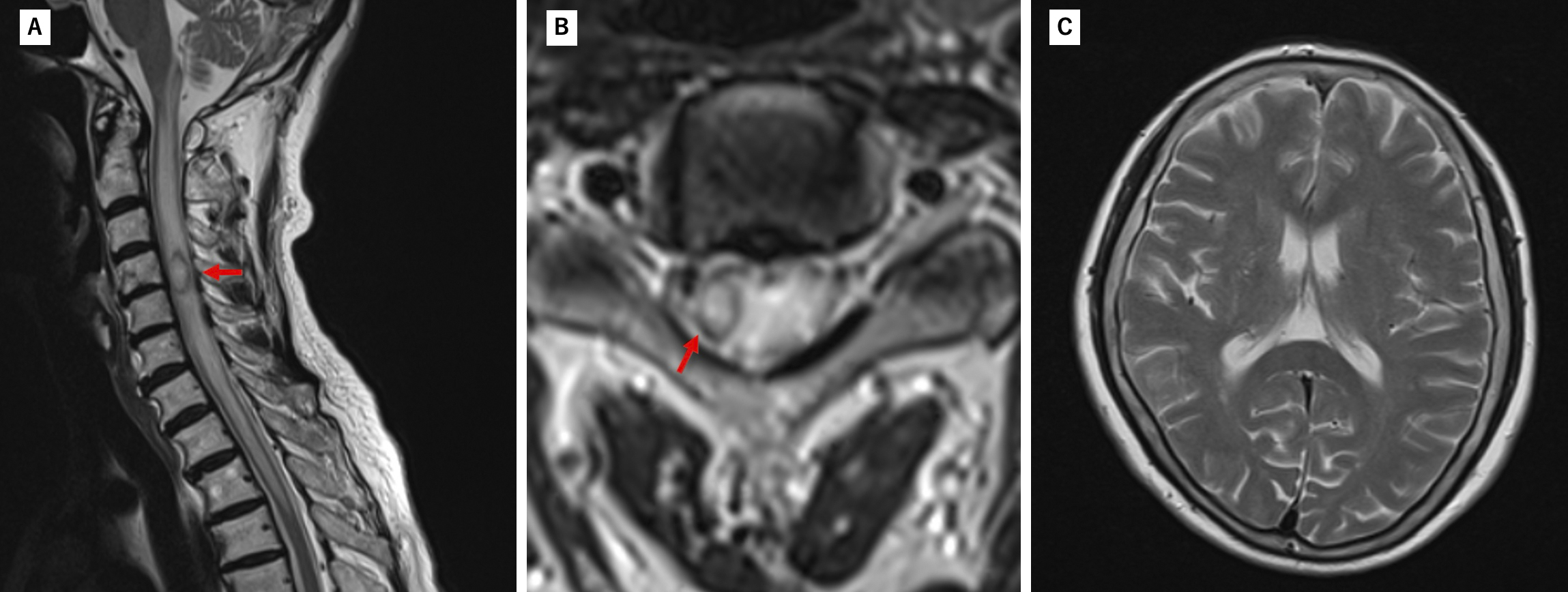
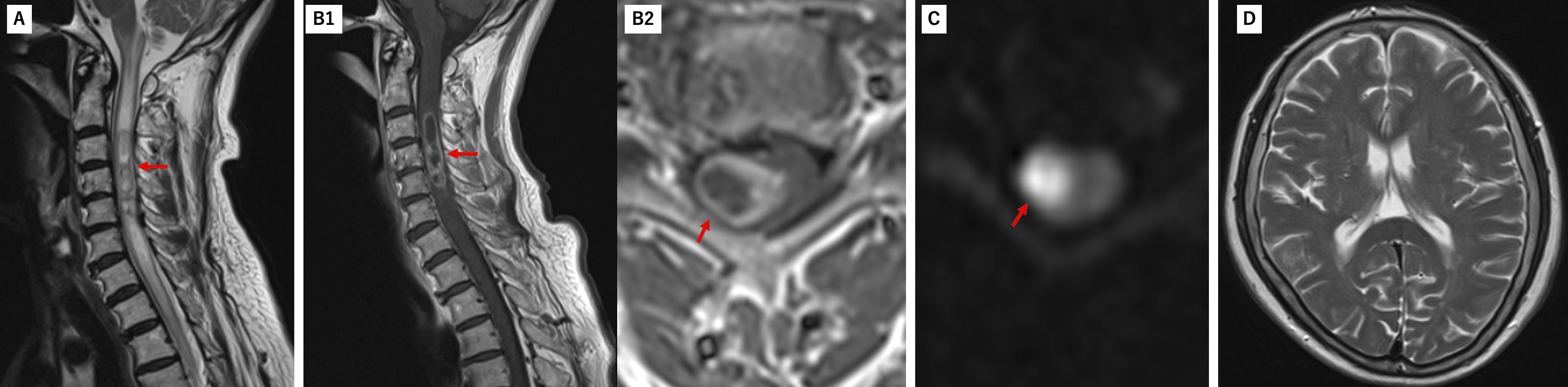
Figure 2. On the second day of hospitalization, a follow-up MRI showed progressive lesion expansion (red arrow) with worsening edema and ring-like enhancement on contrast-enhanced MRI, and high signal intensity on diffusion-weighted imaging in the same region. Brain MRI showed no changes compared to admission, with no hydrocephalus or findings suggestive of brain abscess or ventriculitis. (A: T2WI Sagittal; B1, 2: gadolinium-enhanced T1WI Sagittal, Axial; C: DWI Axial; D: T2WI Axial).
MRI: magnetic resonance imaging; T2WI: T2 weighted image.
From: Rapidly Progressive Impaired Consciousness in Cervical Intramedullary Spinal Cord Abscess: A Case Report
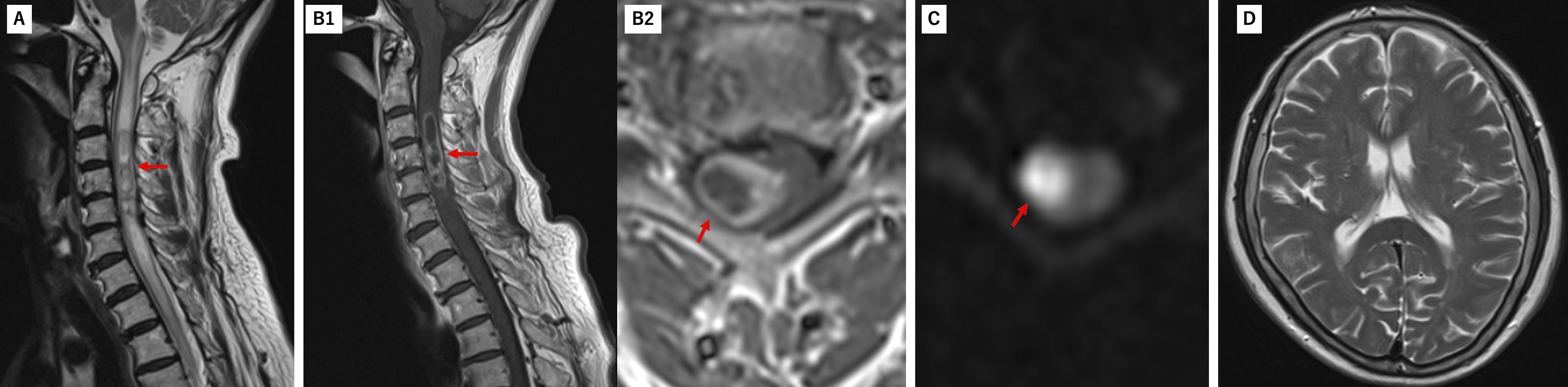
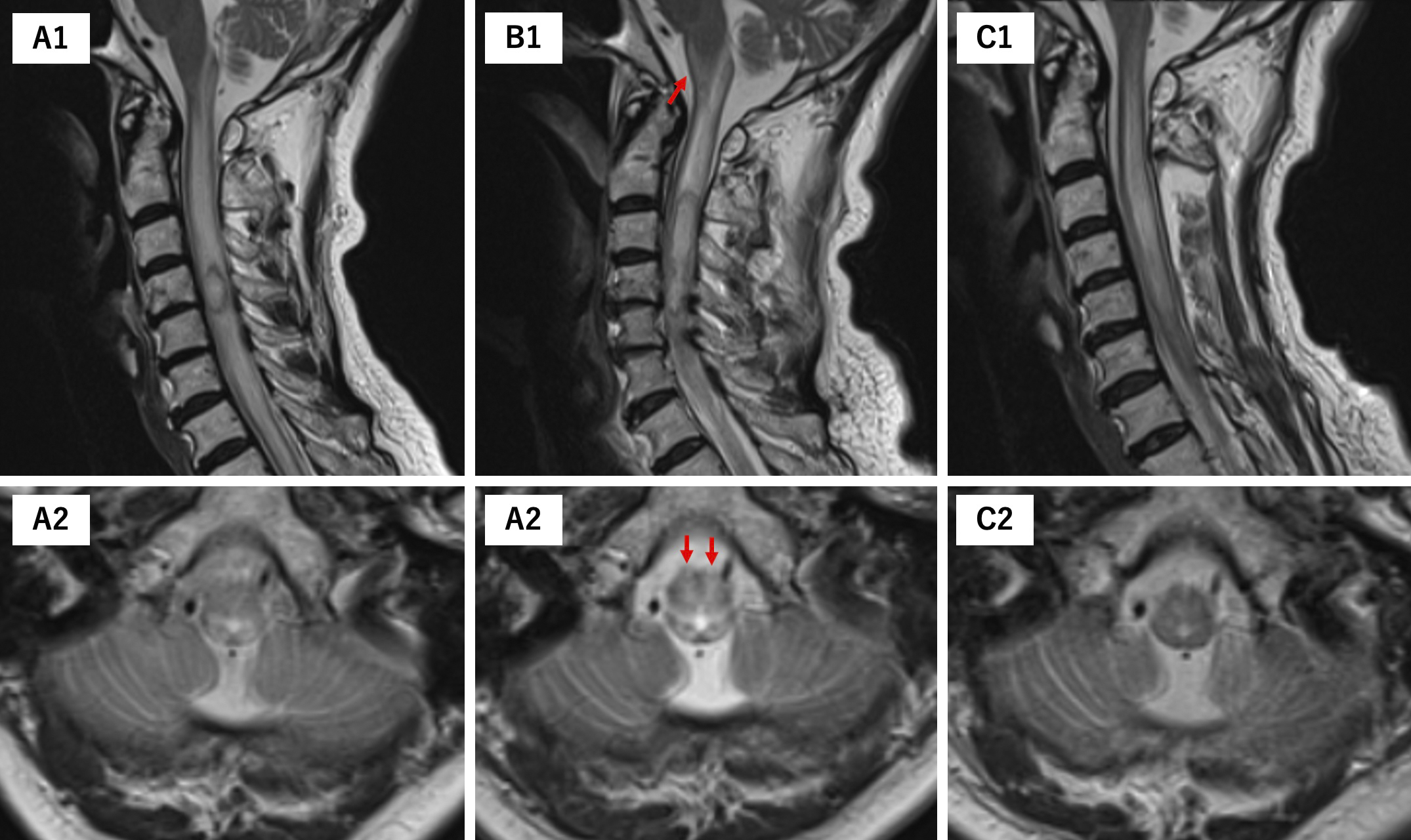
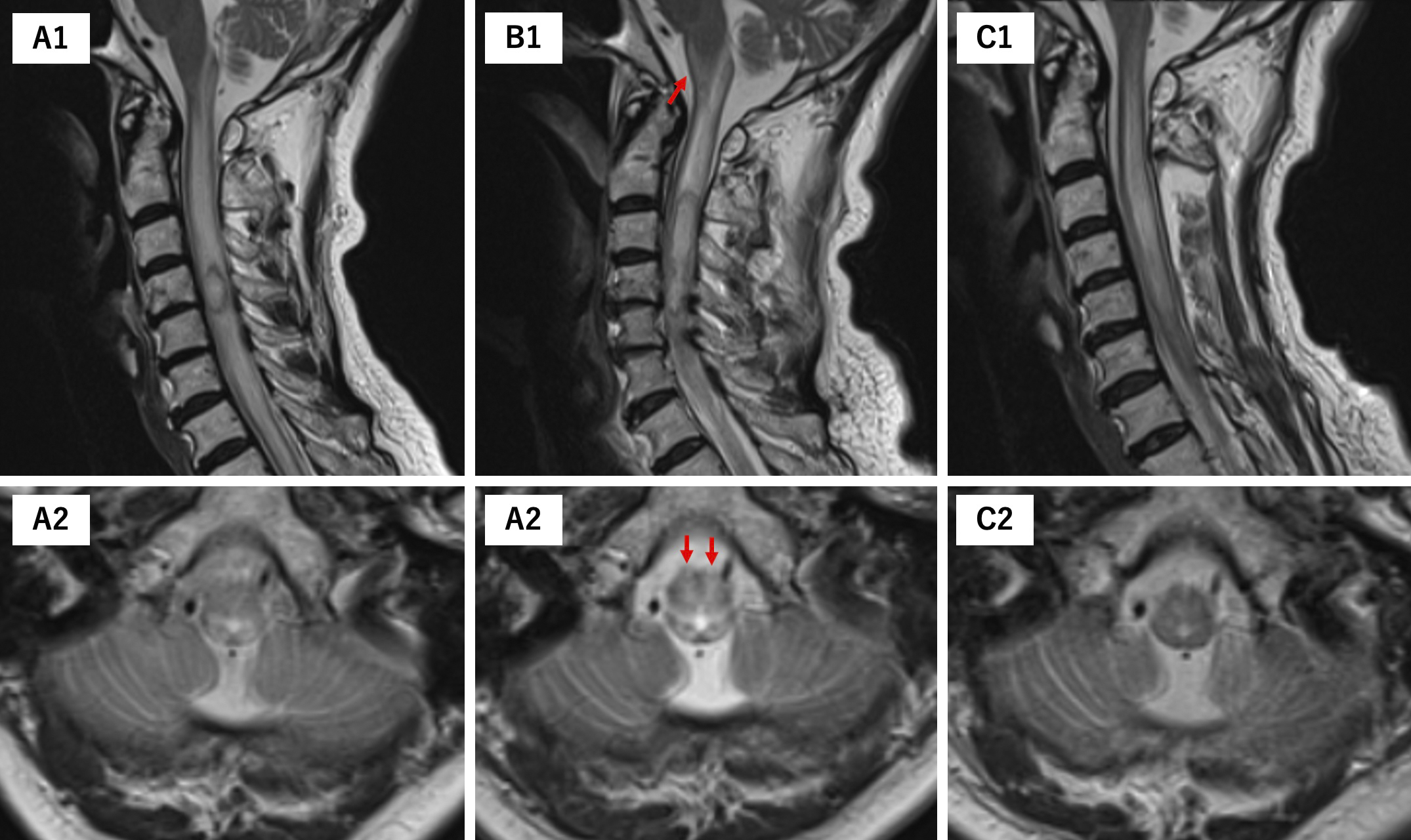
Figure 4. Initial MRI showed edematous changes limited to the dorsal brainstem (A1, 2). When the patient developed impaired consciousness, the MRI revealed that the edema had spread to the central and ventral medulla (red arrows) (B1, 2). Postoperative imaging showed improvement in brainstem edema (C1, 2), which was accompanied by recovery of consciousness. (A1, B1, C1: T2WI Sagittal; A2, B2, C2: T2WI Axial). MRI: magnetic resonance imaging; T2WI: T2 weighted image.
From: Rapidly Progressive Impaired Consciousness in Cervical Intramedullary Spinal Cord Abscess: A Case Report