Corresponding author: Hideto Oshita, oshita1978@gmail.com
DOI: 10.31662/jmaj.2020-0002
Received: January 15, 2020
Accepted: July 20, 2020
Advance Publication: October 2, 2020
Published: October 15, 2020
Cite this article as:
Oshita H, Ito N, Senoo M, Funaishi K, Mitama Y, Okusaki K. The STOP-Bang Test Is Useful for Predicting the Severity of Obstructive Sleep Apnea
. JMA J. 2020;3(4):347-352.
Introduction: The STOP-Bang test was used to detect patients at high risk of obstructive sleep apnea (OSA). We evaluated the usefulness of the STOP-Bang test for predicting the severity of OSA in Japanese patients.
Methods: We retrospectively evaluated the patients who performed full polysomnography at the Mihara Medical Association Hospital. We evaluated the correlation between the STOP-Bang score and the apnea hypopnea index (AHI) using Spearman's rank correlation analysis. We then used multivariate analyses to examine the independent risk factor for severe OSA (AHI ≥ 30/hr).
Results: One hundred seven patients were diagnosed as no (n = 5), mild (n = 17), moderate (n = 30), and severe (n = 55) OSA. The median age was 67 years old (range: 35-84), and 73 of the 107 patients were males. The correlation coefficient between the STOP-Bang score and AHI was 0.701 (P < 0.001). A STOP-Bang score ≥ 5 had sensitivity of 80.0% and specificity of 76.9% for detecting severe OSA. A STOP-Bang score ≥ 5 and BMI ≥ 30 kg/m2 were the independent risk factor for severe OSA.
Conclusions: The STOP-Bang score correlates with AHI and is useful for predicting OSA severity. Polysomnography should be performed actively for the patients with high STOP-Bang scores.
Key words: obstructive sleep apnea, sleep-disordered breathing, STOP-Bang test, apnea hypopnea index
Obstructive sleep apnea (OSA) is a common public health problem, and it has been shown to be associated with an increased incidence of hypertension (1), cardiovascular disease (2) and cerebrovascular disease (3). In addition, OSA is associated with an increased risk of traffic accidents and work-related injuries (4). Diagnosing latent OSA is clinically relevant because untreated OSA has been associated with increased mortality (5).
The STOP-Bang test, developed in 2008 by Chung F. et al., has been widely known as a sensitive, simple and easy-to-remember screening tool for OSA (6). The STOP-Bang acronym stands for: snoring history, tired during the day, observed stop of breathing while sleeping, high blood pressure, BMI > 35 kg/m2 (or 30 kg/m2), age > 50 years, neck circumference > 40 cm and male gender (Table 1). The STOP-Bang test was originally established to screen for OSA in a Canadian surgical population and has been used and validated in a preoperative population (7), sleep clinic population (8), (9), bus-driver population (10) and general population (11) to detect patients at high risk of OSA. Recently, we reported that the Japanese translated version of the STOP-Bang test was useful for risk assessment of OSA in Japanese inpatients (12).
Table 1. The STOP-Bang Test.
| Yes | No | |
|---|---|---|
| STOP | ||
| Do you snore loudly (louder than talking or loud enough to be heard through closed doors)? | 1 | 0 |
| Do you often feel tired, fatigued, or sleepy during daytime? | 1 | 0 |
| Has anyone observed you stop breathing during your sleep? | 1 | 0 |
| Do you have or are you being treated for high blood pressure? | 1 | 0 |
| BANG | ||
| BMI > 30 kg/m2 (or 35 kg/m2)? | 1 | 0 |
| Age over 50 years old? | 1 | 0 |
| Neck circumference > 40 cm? | 1 | 0 |
| Gender: male? | 1 | 0 |
| Total of scores (out of 8) | ||
Although there are several reports on the relationship between the STOP-Bang test and OSA severity, such a relationship has not been as well validated as the usefulness of this test in OSA screening. The purpose of this study was to validate the correlation between the STOP-Bang score and AHI and the detectability of the severe OSA in Japanese.
The population of this retrospective study consisted of consecutive subjects who underwent full polysomnography (PSG) for diagnosis of OSA between April 2017 and June 2019 at the Department of Internal Medicine, the Mihara Medical Association Hospital. The clinical data were collected from electronic medical records. The ethics committee of the Mihara Medical Association Hospital approved this study (no. 291201), and written informed consent was obtained from the patients.
The questionnaire including demographic information (age and gender), symptoms (snoring, apnea, and daytime drowsiness) and comorbidities (hypertension, diabetes mellitus, hyperlipidemia, cardiovascular disease, and cerebrovascular disease) was filled by all subjects. Anthropometric parameters (body weight, height, and neck circumference) were measured by a nurse or doctor. The Epworth sleepiness scale (ESS) is an eight-item questionnaire used to measure daytime sleepiness. The questionnaire has a four-point Likert response format, and the score ranges from 0 to 24. ESS score ≥ 11 indicates excessive daytime sleepiness and high risk of OSA (13). Contents of the Japanese translated version of the STOP-Bang test (14) and ESS were mixed into the questionnaire, and STOP-Bang score and ESS were calculated after the diagnosis process was completed. We used 30 kg/m2 as the cutoff value for BMI according to previous studies in the Asian population (9), (12), (15).
PSG (PSG-1100, Nihon Kohden) included recordings of six electroencephalogram channels: bilateral electro-oculograms, chin and tibialis electromyogram, electrocardiogram, airflow by nasal pressure transducer and oronasal thermocouples, chest and abdominal wall motion by piezo electrodes, and oxygen saturation by pulse oximeter. Respiratory events were manually scored according to the American Association of Sleep Medicine guideline 2015 (16) by the clinical laboratory technician using the dedicated software. AHI was defined as the total number of apneas and hypopneas per hour of sleep. The severity of OSA based upon the AHI was categorized into four groups: none (AHI < 5/h), mild (5 ≤ AHI < 15/h), moderate (15 ≤ AHI < 30/h), and severe (AHI ≥ 30/h).
The patients were divided by presence or absence of severe OSA, and clinical features obtained from the questionnaire were compared. We present continuous variables as median and range and categorical variables as numbers and percentages. We compared continuous variables by Wilcoxon rank-sum test. We compared categorical variables using the χ2 test when appropriate; otherwise, we used Fisher’s exact test.
The receiver operating characteristic (ROC) curve analysis was performed to evaluate the diagnostic value of the STOP-Bang test for detecting severe OSA and determining the best cutoff value. We used Spearman's rank method to examine the correlation between the STOP-Bang score or ESS and AHI. To detect the independent risk factor of severe OSA, we performed multivariate logistic regression analyses with backward elimination using the categorical variables that had shown statistical significance in univariate analyses.
All analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) (17), a graphical user interface for R statistical programming software (The R Foundation, Vienna, Austria). We regarded a P value under 0.05 as statistically significant.
One hundred nine subjects underwent full PSG as diagnosis for OSA during the inclusion period. Two subjects were excluded because of lack of clinical data (n = 1) and diagnosis of central sleep apnea (n = 1). Therefore, 107 patients were finally included in our study and categorized into 4 groups: no (n = 5), mild (n = 17), moderate (n = 30), and severe (n = 55) OSA on the basis of AHI.
In the study population, the median age of 67 years (range 35-84 years), and 68.2% of the patients were males, with median BMI of 26.4 kg/m2 (range: 17.3-42.3 kg/m2), and a with median neck circumference of 38.5 cm (range: 31-47 cm). Descriptive characteristics of the study and comparison between the patients with and without severe OSA are displayed in Table 2. The patients with severe OSA had a higher BMI and thicker neck circumference than the patients without severe OSA. They also had a higher prevalence of hypertension, hyperlipidemia and OSA symptoms such as snoring and apnea. The STOP-Bang score was significantly higher in the patients with severe OSA.
Table 2. Characteristics of the Study Population and Comparison between the Patients with Mild-to-moderate OSA and Those with Severe OSA.
| Total | Without severe OSA | With severe OSA | P value | |
|---|---|---|---|---|
| n | 107 | 52 | 55 | |
| Continuous variables, median [range] | ||||
| Age, years old | 67 [35–84] | 64 [35–81] | 69 [35–84] | 0.02 |
| Height, cm | 164.0 [141.0–181.2] | 164.0 [141.0–181.2] | 164.0 [142.0–180.0] | 0.87 |
| Body weight, kg | 69.0 [42.0–118.0] | 64.6 [42.0–103.0] | 73.2 [45.0–118.0] | 0.002 |
| BMI, kg/m2 | 26.4 [17.3–42.3] | 23.9 [17.3–40.6] | 28.3 [17.7–42.3] | < 0.001 |
| Neck circumference, cm | 38.5 [31.0–47.0] | 38.0 [31.0–43.0] | 40.0 [32.0–47.0] | < 0.001 |
| Apnea hypopnea index, /hr | 31.0 [1.9–75.9] | 16.5 [1.9–27.9] | 48.6 [30.5–75.9] | < 0.001 |
| Epworth sleepiness scale | 6 [0–22] | 6 [0–22] | 7 [0–21] | 0.17 |
| STOP-Bang score | 5 [2–8] | 3.5 [2–7] | 5 [2–8] | < 0.001 |
| Categorical variables, n (%) | ||||
| Male | 73 (68.2) | 33 (63.5) | 40 (72.7) | 0.41 |
| Age ≧ 50 years old | 97 (90.7) | 45 (86.5) | 52 (94.5) | 0.19 |
| BMI≧30 kg/m2 | 34 (31.8) | 8 (15.4) | 26 (47.3) | < 0.001 |
| Neck circumference ≧ 40cm | 39 (36.4) | 11 (21.2) | 28 (50.9) | 0.002 |
| Tired during the day | 61 (57.5) | 26 (50.0) | 35 (64.8) | 0.17 |
| Snoring history (%) | 70 (65.4) | 27 (51.9) | 43 (78.2) | 0.005 |
| Observed apnea while asleep | 40 (37.7) | 13 (25.0) | 27 (50.0) | 0.01 |
| Hypertension | 71 (66.4) | 29 (55.8) | 42 (76.4) | 0.03 |
| Hyperlipidemia | 50 (46.7) | 18 (34.6) | 32 (58.2) | 0.02 |
| Diabetes mellitus | 39 (36.4) | 19 (36.5) | 20 (36.4) | 1 |
| Cardiovascular disease | 25 (23.4) | 13 (25.0) | 12 (21.8) | 0.82 |
| Cerebrovascular disease | 10 (9.3) | 5 (9.6) | 5 (9.1) | 1 |
| STOP-Bang score ≧ 5 | 56 (52.3) | 12 (23.1) | 44 (80.0) | < 0.001 |
| BMI, body mass index; OSA, obstructive sleep apnea | ||||
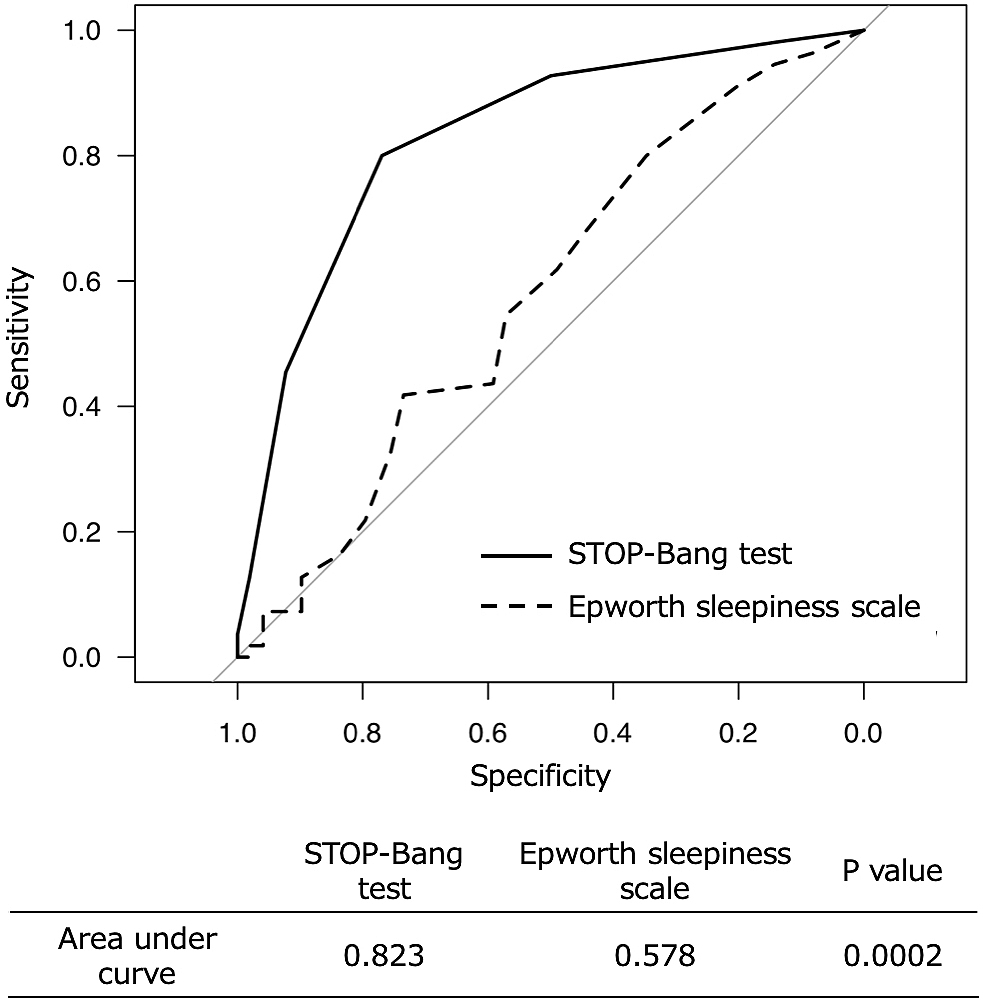
In Figure 1, we presented the ROC curves of the STOP-Bang test and ESS for detecting severe OSA. The STOP-Bang test showed statistically significantly higher area under curve (AUC) than ESS. We determined the best cutoff value to be five points of the STOP-Bang score for detecting severe OSA and resulted in sensitivity of 80% and specificity of 76.9%.
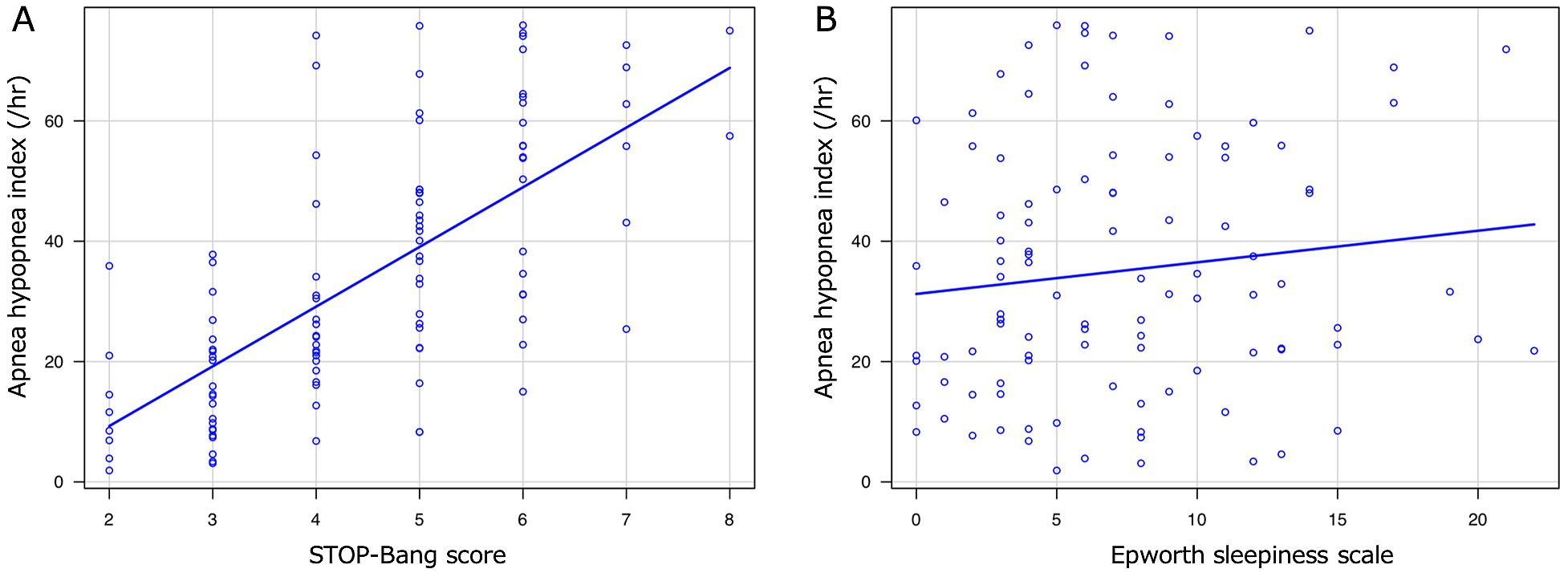
The AHI of the patients according to their STOP-Bang score and ESS are presented in Figure 2. The Spearman's rank sum test showed significantly correlation between the STOP-Bang score and AHI (correlation coefficient: 0.701, P < 0.001).
Finally, we performed multivariate logistic regression analyses with backward elimination using a STOP-Bang score ≥ 5, BMI ≥ 30 kg/m2, hypertension, hyperlipidemia, observed apnea while sleeping, neck circumference ≥ 40 cm, and snoring history and found that the STOP-Bang score ≥ 5 and BMI ≥ 30 kg/m2 was an independent risk factor of severe OSA (Table 3).
Table 3. The Multivariate Logistic Regression Analyses for Detecting Severe OSA.
| Odds ratio (95% confidence interval) | P value | |
|---|---|---|
| STOP-Bang score ≧ 5 | 11.90 (3.10–45.4) | 0.0003 |
| BMI ≧ 30 kg/m2 | 3.25 (1.03–10.30) | 0.045 |
| Hyperlipidemia | 2.12 (0.78–5.75) | 0.14 |
| Observed apnea while asleep | 2.14 (0.72–6.34) | 0.17 |
| Neck circumference ≧ 40 cm | 0.62 (0.15–2.46) | 0.49 |
| BMI, body mass index; OSA, obstructive sleep apnea | ||
Although OSA is a very common disease, only a few cases are diagnosed and receive treatment. Marin et al. reported that severe-OSA patients have higher incidence of fatal and non-fatal cardiovascular events than mild-moderate-OSA patients (18). Especially, untreated severe OSA patients should get a poor prognosis and be diagnosed and treated as early as possible.
Although the STOP-Bang test is a useful questionnaire for risk assessment of OSA, low specificity and low positive predictive value have been pointed out (19). Because many normal subjects and mild OSA patients also fall under the STOP-Bang ≥ 3, performing full PSG for all subjects with STOP-Bang ≥ 3 might be a waste of effort and cost. Several researchers, therefore, focused on the usefulness of the STOP-Bang test in predicting the severity, not in predicting the presence of OSA. Farney et al. and Chung et al. demonstrated that as the STOP-Bang score increased, the probability of having more severe OSA also increased (20), (21). However, the relationship between the STOP-Bang score and the severity of OSA is not as well established as the usefulness in OSA screening.
In the group of Japanese patients who underwent PSG, our result revealed that the STOP-Bang score correlated well with AHI and suggested that the STOP-Bang test was useful for predicting OSA severity. Notably, the STOP-Bang test was overwhelmingly better than ESS, which is widely used as a sleepiness index, in correlation with AHI and in the diagnostic value of detecting severe OSA. In particular, the STOP-Bang score > 5 showed sufficient diagnostic value in the detection of severe OSA. A high STOP-Bang score could have the clinical significance that PSG should be performed preferentially.
We recognize that this study has several limitations. First, it is a single-center study, and the number of cases might not be sufficient to generalize the results. Validation in another large cohort is required. Second, this study evaluated only patients who underwent PSG on their own will because of suspected OSA based on symptoms or physical features. This causes the selection bias, and the results cannot be easily generalized to subjects who are not concerned about their sleep.
Despite several limitations, our results suggest that the STOP-Bang test can estimate the OSA severity, and PSG should be strongly recommended for a patient with a high STOP-Bang score. The STOP-Bang test is a tool that many clinicians should know to find poor prognostic OSA patients early.
None
Hideto Oshita conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
Noriaki Ito, Misato Senoo, and Kunihiko Funaishi coordinated the data collection and approved the final manuscript as submitted.
Yasuyuki Mitama and Ken Okusaki supervised this study, critically reviewed the manuscript, and approved the final manuscript as submitted.
The study was approved by the Ethics Committee of the Mihara Medical Association Hospital (approval code: 291201).
Kales A, Bixler EO, Cadieux RJ, et al. Sleep apnoea in a hypertensive population. Lancet. 1984;2(8410):1005-8.
Yumino D, Tsurumi Y, Takagi A, et al. Impact of obstructive sleep apnea on clinical and angiographic outcomes following percutaneous coronary intervention in patients with acute coronary syndrome. Am J Cardiol. 2007;99(1):26-30.
Johnson KG, Johnson DC. Frequency of sleep apnea in stroke and TIA patients: A meta-analysis. J Clin Sleep Med. 2010;6(2):131-7.
Hirsch Allen AJM, Bansback N, Ayas NT. The effect of OSA on work disability and work-related injuries. Chest. 2015;147(5):1422-8.
He J, Kryger MH, Zorick FJ, et al. Mortality and apnea index in obstructive sleep apnea. Experience in 385 male patients. Chest. 1988;94(1):9-14.
Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: A tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812-21.
Nunes FS, Danzi-Soares NJ, Genta PR, et al. Critical evaluation of screening questionnaires for obstructive sleep apnea in patients undergoing coronary artery bypass grafting and abdominal surgery. Sleep Breath. 2015;19(1):115-22.
Reis R, Teixeira F, Martins V, et al. Validation of a Portuguese version of the STOP-Bang questionnaire as a screening tool for obstructive sleep apnea: Analysis in a sleep clinic. Rev Port Pneumol. 2015;21(2):61-8.
Ong TH, Raudha S, Fook-Chong S, et al. Simplifying STOP-BANG: Use of a simple questionnaire to screen for OSA in an Asian population. Sleep Breath. 2010;14(4):371-6.
Firat H, Yuceege M, Demir A, et al. Comparison of four established questionnaires to identify highway bus drivers at risk for obstructive sleep apnea in Turkey. Sleep Biol Rhythms. 2012;10(3):231-6.
Silva GE, Vana KD, Goodwin JL, et al. Identification of patients with sleep disordered breathing: Comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth sleepiness scales. J Clin Sleep Med. 2011;7(5):467-72.
Oshita H, Fuchita H, Ito N, et al. [Validation of the Japanese version of the STOP-Bang test for the risk assessment of obstructive sleep apnea syndrome]. Journal of Japan Primary Care Association. 2019;42(1):26-31. Japanese.
Johns MW. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep. 1991;14(6):540-5.
Inagaki Y. [Perioperative anesthetic management of the patients with obstructive sleep apnea syndrome]. Journal of Japanese Society of Stomato-pharyngology. 2017;30(1):9-16. Japanese.
Kim B, Lee EM, Chung YS, et al. The utility of three screening questionnaires for obstructive sleep apnea in a sleep clinic setting. Yonsei Med J. 2015;56(3):684-90.
Berry RB, Gamaldo CE, Harding SM, et al. AASM Scoring manual version 2.2 updates: New chapters for scoring infant sleep staging and home sleep apnea testing. J Clin Sleep Med. 2015;11(11):1253-4.
Kanda Y. Investigation of the freely-available easy-to-use software “EZR” (Easy R) for medical statistics. Bone Marrow Transplant. 2013;48(3):452-8.
Marin JM, Carrizo SJ, Vicente E, et al. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet. 2005;365(9464):1046-53.
Kørvel-Hanquist A, Andersen IG, Lauritzen E, et al. Validation of the Danish STOP-Bang obstructive sleep apnoea questionnaire in a public sleep clinic. Dan Med J. 2018;65(1):1-5.
Farney RJ, Walker BS, Farney RM, et al. The STOP-Bang equivalent model and prediction of severity of obstructive sleep apnea: Relation to polysomnographic measurements of the apnea/hypopnea index. J Clin Sleep Med. 2011;7(5):459-65B.
Chung F, Subramanyam R, Liao P, et al. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012;108(5):768-75.