Corresponding author: Yoshinosuke Shimamura, yshimamura.tkh@gmail.com
DOI: 10.31662/jmaj.2021-0064
Received: April 10, 2021
Accepted: June 4, 2021
Advance Publication: September 1, 2021
Published: October 15, 2021
Cite this article as:
Shimamura Y, Ogawa Y, Takizawa H. Chilblain Lupus Erythematosus. JMA J. 2021;4(4):423-425.
Key words: Chilblain lupus erythematosus, systemic lupus erythematosus, proteinuria, hematuria
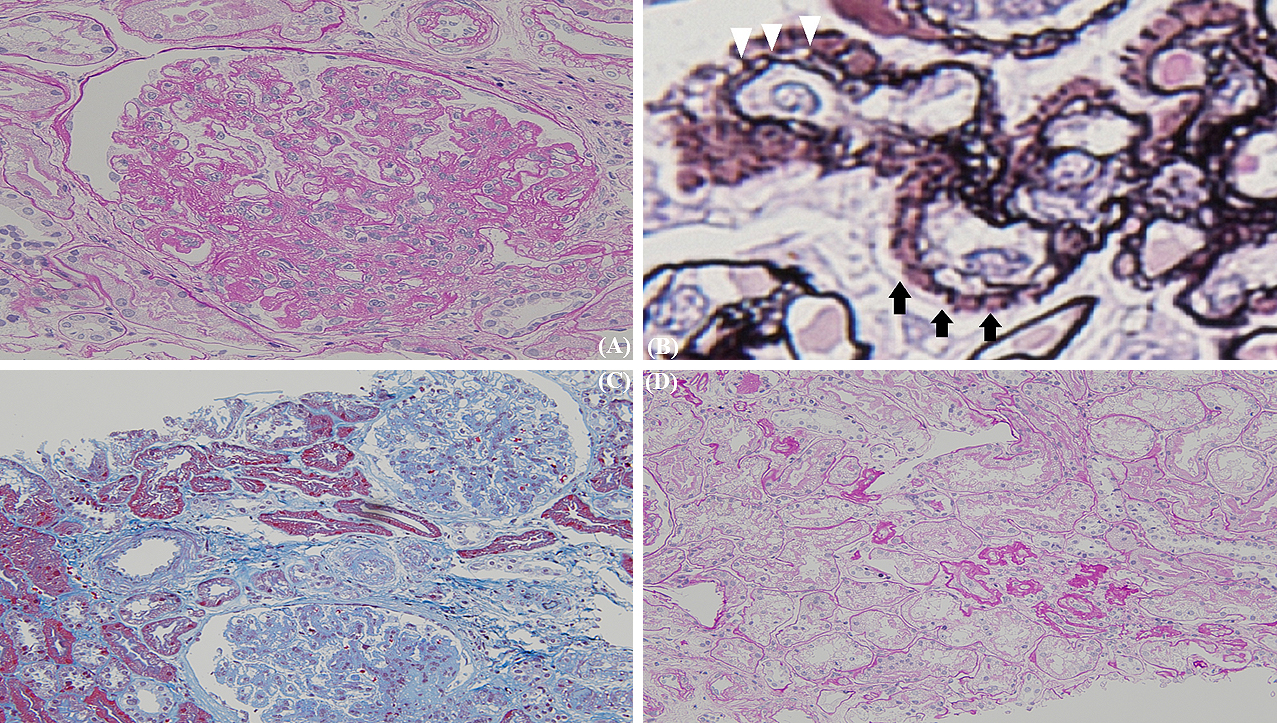
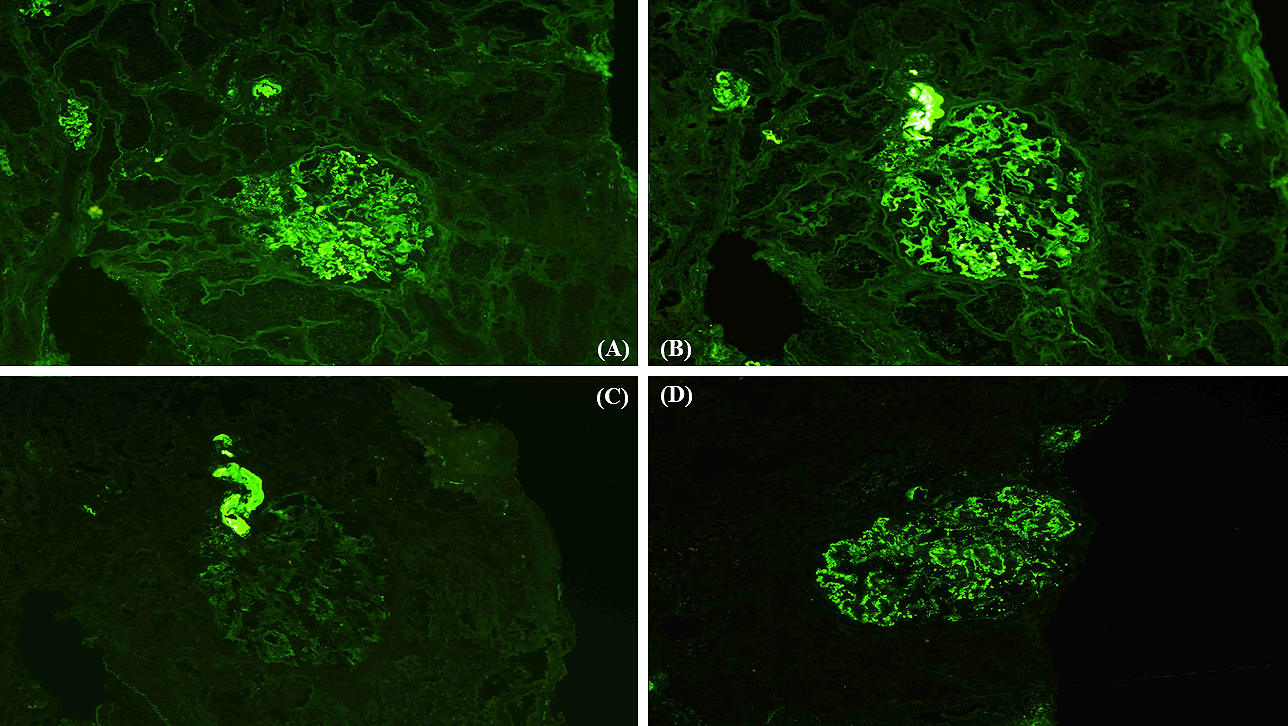
A 41-year-old man presented with a painful rash on his fingers for the last 6 months. He had a history of digital amputation. Notable findings included papuloerythematous plaques on the back of his palms and fingers (Figure 1). Urinalysis revealed proteinuria and microhematuria. The patient was positive for antinuclear (speckled pattern), anti-double-stranded DNA, and anti-Smith antibodies and negative for cryoglobulin and antiphospholipid antibodies. Renal biopsy (Figures 2 and 3) confirmed the diagnosis of systemic lupus erythematosus (SLE) presenting with chilblain lupus erythematosus (CLE) and lupus nephritis class III (A/C) and V as per the Renal Pathology Society/International Society of Nephrology classification. Six months after the initiation of prednisolone and mycophenolate mofetil, proteinuria and hematuria disappeared and the skin rash improved.
CLE is one of the forms of skin manifestations of SLE (1), is characterized by painful papuloerythematous plaques over the fingers (2), (3), and can be mistakenly diagnosed as chilblain (3). Physicians should be aware of CLE because it can be the initial manifestation of SLE and may require further investigation to determine other organ involvement in SLE (2), (3).

None
We would like to thank Editage (www.editag.jp) for English language editing.
Conceptualization YS, HT; Investigation YS, HT; Project administration HT; Resources YO; Supervision HT; Visualization YO; Writing - original draft YS, YO, HT; Writing - review & editing YS, YO, HT.
2-020083-00 issued by the institutional review board at the Teine Keijinkai Medical Center
Written informed consent was obtained from all patients to publish the information, including their photographs.
Aringer M, Costenbader K, Daikh D, et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 2018;71(9):1400-12.
Obermoser G, Sontheimer RD, Zelger B. Overview of common, rare, and atypical manifestations of cutaneous lupus erythematosus and histopathological correlates. Lupus. 2020;19(9):1050-70.
Hedrich CM, Fiebig B, Hauck FH, et al. Chilblain lupus erythematosus―a review of literature. Clin Rheumatol. 2008;27(8):949-54.