Corresponding author: Takahiko Kinjo, kinjo1984@gmail.com
DOI: 10.31662/jmaj.2024-0194
Received: July 26, 2024
Accepted: August 30, 2024
Advance Publication: November 1, 2024
Published: January 15, 2025
Cite this article as:
Kinjo T, Hamaura S, Tomita H. Hypotensive Dumping Syndrome in Hypertrophic Obstructive Cardiomyopathy. JMA J. 2025;8(1):295-297.
Key words: hypertrophic obstructive cardiomyopathy, dumping syndrome, distributive shock, nasogastric tube malposition
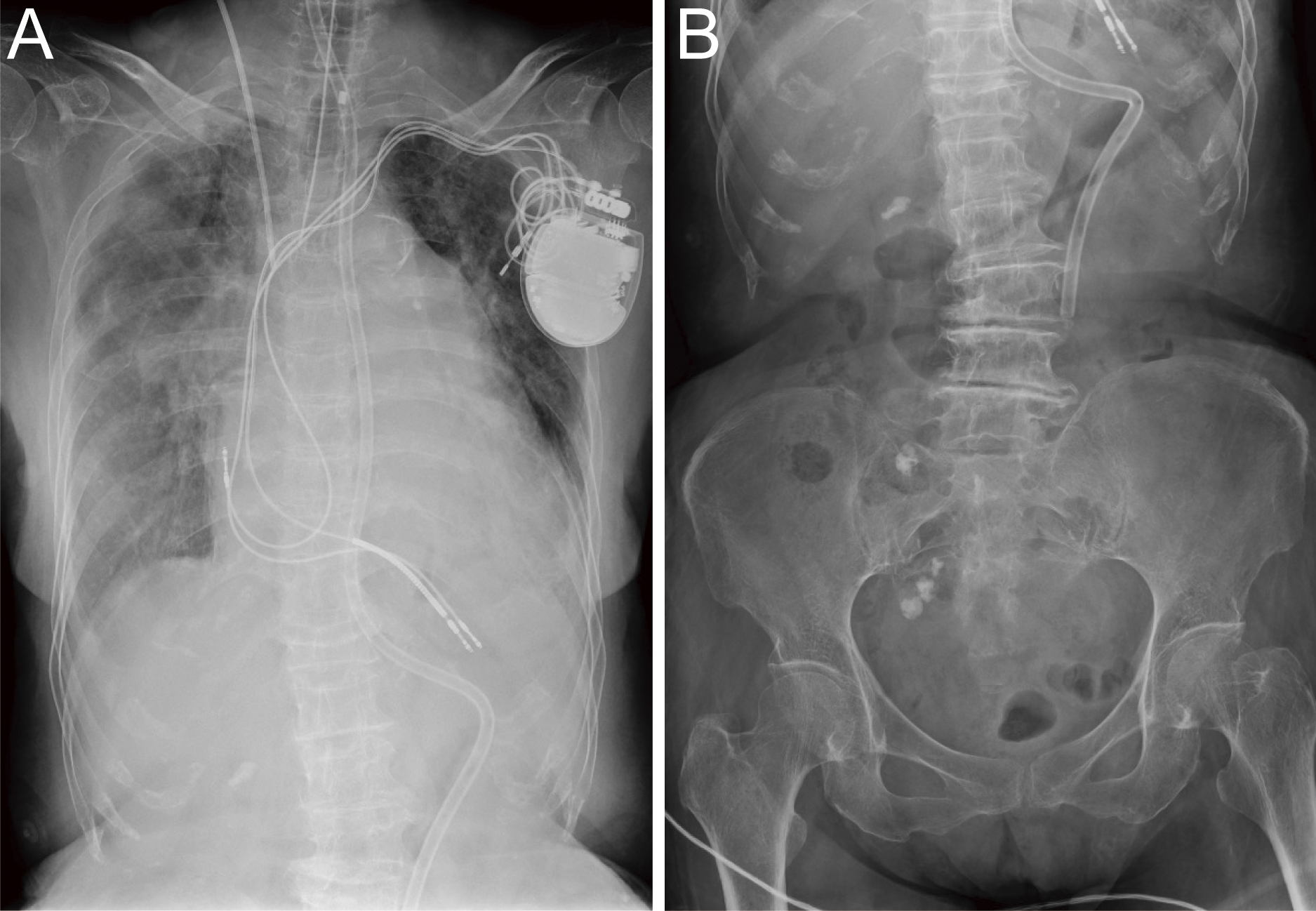
A 79-year-old woman with hypertrophic obstructive cardiomyopathy (HOCM) (Figure 1) was admitted for pneumonia (Figure 2) and require intubation and mechanical ventilation. Severe hypotension with restlessness was reproducibly induced 30 min after feeding using a nasogastric tube. We diagnosed the patients with early dumping syndrome because gastrointestinal radiography revealed that the nasogastric tube tip was positioned at the gastric pylorus (Figure 3), whereas the duodenum was immediately contrasted. Post-feeding hypotension no longer occurred after the tube tip was pulled back into the gastric body. Dumping syndrome without previous gastric surgery was also reported when a nasogastric tube (1) or gastrostomy tube (2) was positioned in the duodenum.

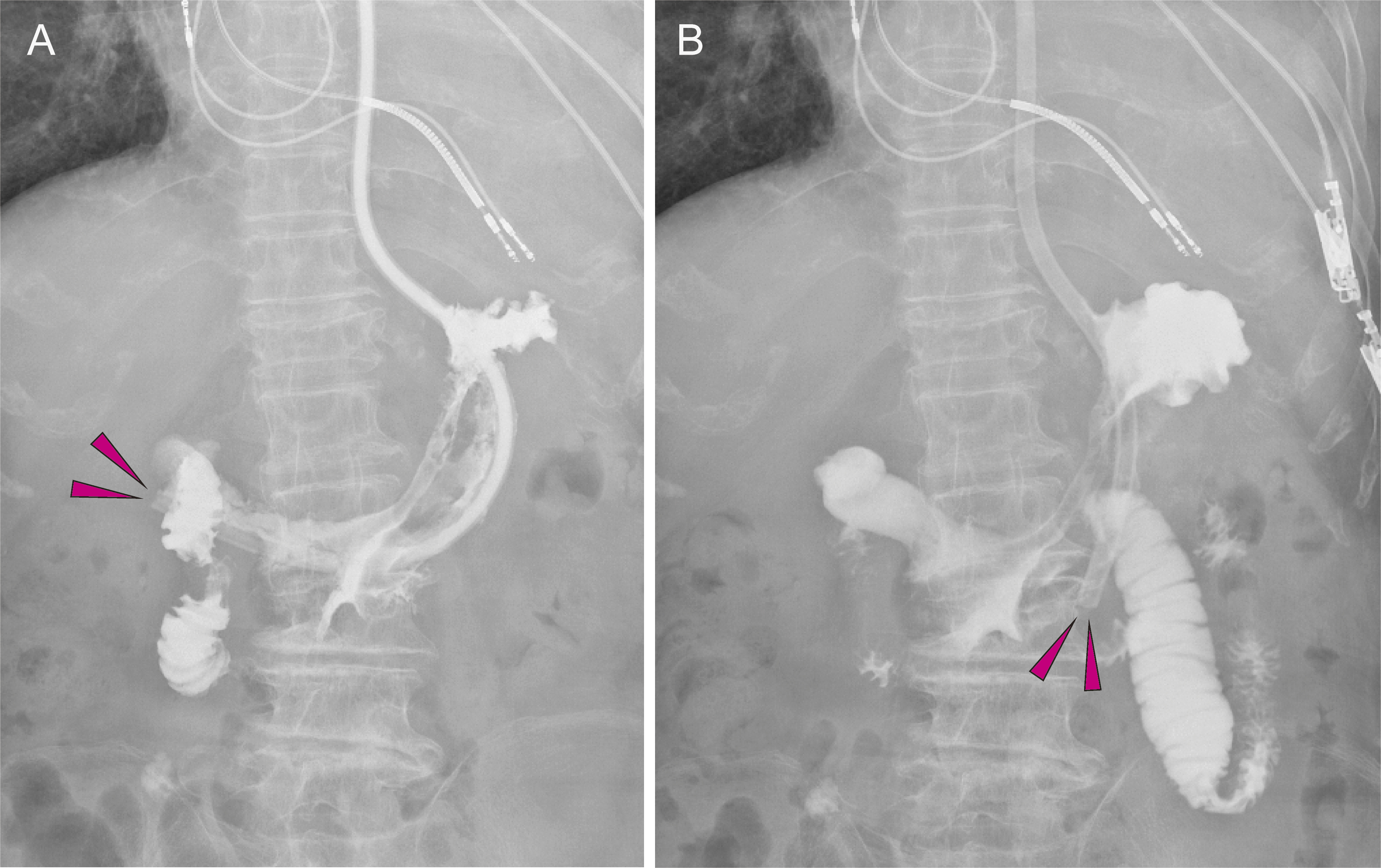
Reduction of preload and vasodilation exacerbates left ventricular outflow obstruction in patients with HOCM (3). Early dumping syndrome, which is characterized by rapid flushing of the hyperosmolar feed into the intestine and subsequent fluid distribution and vasodilation, may cause severe hypotension in patients with HOCM.
Dr. Hirofumi Tomita is a concurrent professor of the Department of Advanced Management of Cardiac Arrhythmias and received a research grant from Abbott Medical Japan LLC. Other authors have no relevant disclosures.
TK conceived the study and wrote the manuscript. All authors contributed to patient care and to editing the manuscript.
An IRB approval is not required because this is a case report.
The patient gave informed consent to publish this case report.
Data sharing does not apply to this article because no datasets were generated or analyzed during this report.
Allen DB. Postprandial hypoglycemia resulting from nasogastric tube malposition. Pediatrics. 1988;81(4):582-4.
Shimoda M, Saraya T, Ogawa Y, et al. Dumping syndrome due to the misplacement of the gastrostomy feeding tube. Intern Med. 2015;54(19):2529.
Kitaoka H, Tsutsui H, Kubo T, et al. JCS/JHFS 2018 guideline on the diagnosis and treatment of cardiomyopathies. Circ J. 2021;85(9):1590-689.