Corresponding author: Tomoyuki Fujioka, fjokmrad@tmd.ac.jp
DOI: 10.31662/jmaj.2024-0239
Received: September 8, 2024
Accepted: November 14, 2024
Advance Publication: January 31, 2025
Published: April 28, 2025
Cite this article as:
Yamaga E, Fujioka T, Katsuta L, Hayashi M, Yamamuro K, Kumaki Y, Hayashi K, Oda G, Kubota K, Tateishi U. Detecting Breast Cancer via Innovative Magnetic Resonance Elastography with External Vibrations to the Back. JMA J. 2025;8(2):596-598.
Key words: breast cancer, magnetic resonance imaging (MRI), magnetic resonance elastography (MRE)
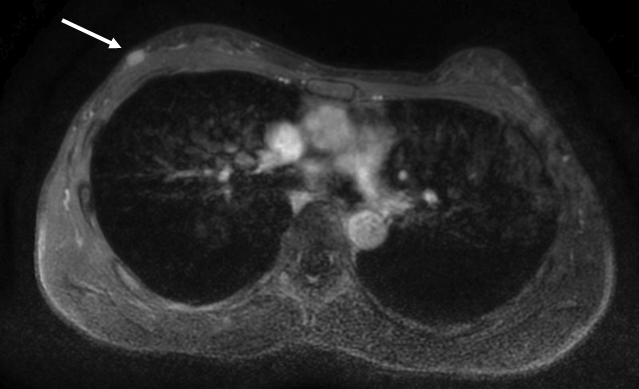
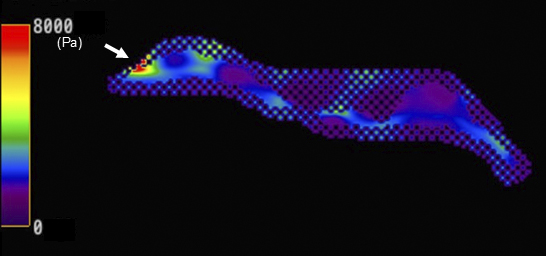
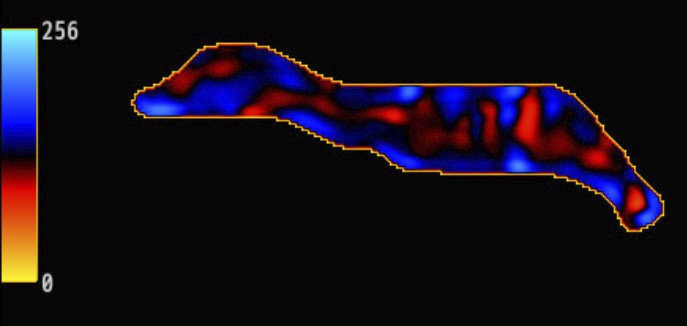
A woman in her 40s, with a mass detected in her right breast through screening ultrasound, underwent breast magnetic resonance elastography (MRE); the results revealed a hard, elastic mass, which was later confirmed as invasive ductal carcinoma (Figure 1, 2 and 3). The patient received hormone therapy after surgery and remains relapse-free since then. Elastography measures tissue stiffness by assessing the propagation of external vibrations and is implemented using ultrasound and magnetic resonance imaging (1). Although MRE is clinically used to assess liver cirrhosis, its application for breast imaging remains unclear (2). Previous reports required specialized devices to apply external vibrations directly to the breast for performing breast MRE (3), (4). However, we have developed a simplified approach that enables breast MRE by applying external vibrations from the back using a passive driver originally designed for liver applications (Figure 4). This method considerably contributed to a highly confident diagnosis of breast cancer.

None
This work was supported by JSPS KAKENHI grant number JP21K15842.
We used GPT-4 (https://chat.openai.com/) for Japanese to English translation and English proofreading. The generated text was reviewed, revised, and proofread by the authors. We would like to express our gratitude to “Irasutoya” for allowing us to use their illustrations in this paper.
All the authors cared for the patient, as well as wrote and approved the final manuscript.
The Ethics Review Committee of the Faculty of Medicine, Institute of Science Tokyo approved this study (approval number: M2020-206). All procedures performed involving the patient were in accordance with the ethical standards of the institutional and/or National Research Committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent was obtained from the patient.
Muthupillai R, Lomas DJ, Rossman PJ, et al. Magnetic resonance elastography by direct visualization of propagating acoustic strain waves. Science. 1995;269(5232):1854-7.
Moura Cunha G, Fan B, Navin PJ, et al. Interpretation, reporting, and clinical applications of liver MR elastography. Radiology. 2024;310(3):e231220.
Bohte AE, Nelissen JL, Runge JH, et al. Breast magnetic resonance elastography: a review of clinical work and future perspectives. NMR Biomed. 2018;31(10):e3932.
Kim HJ, Kim HH, Choi WJ, et al. Correlation of shear-wave elastography parameters with the molecular subtype and axillary lymph node status in breast cancer. Clin Imaging. 2023;101:190-9.