Corresponding author: Rikuto Christopher Shinohara, rcshinohara@gmail.com
DOI: 10.31662/jmaj.2024-0248
Received: August 28, 2024
Accepted: January 27, 2025
Advance Publication: April 4, 2025
Published: April 28, 2025
Cite this article as:
Shinohara RC, Takayanagi S, Furutaka Y, Watanabe S. Subacute Encephalopathy and Seizures in Alcoholics Syndrome. JMA J. 2025;8(2):617-619.
Key words: alcohol withdrawal, seizure, epilepsy
A 56-year-old male with alcohol dependence, abstinent for 2 days, was brought to the emergency department with generalized tonic-clonic seizures. He had no history of seizure or withdrawal and had discontinued outpatient treatment. Magnetic resonance imaging (MRI) showed focal hyperintensity (Figure 1A-C). Despite treatment with diazepam and lacosamide, he remained unconscious (E1V1M4). By day 4, his consciousness improved (E4V3M5). Electroencephalography (EEG) revealed lateralized periodic discharges (Figure 1D), confirming a diagnosis of subacute encephalopathy with seizures in alcoholics (SESA) syndrome. By day 24, he regained consciousness but had motor aphasia and visual hallucinations. By day 63, his symptoms remitted and he was transferred to rehabilitation (Figure 2A-D).
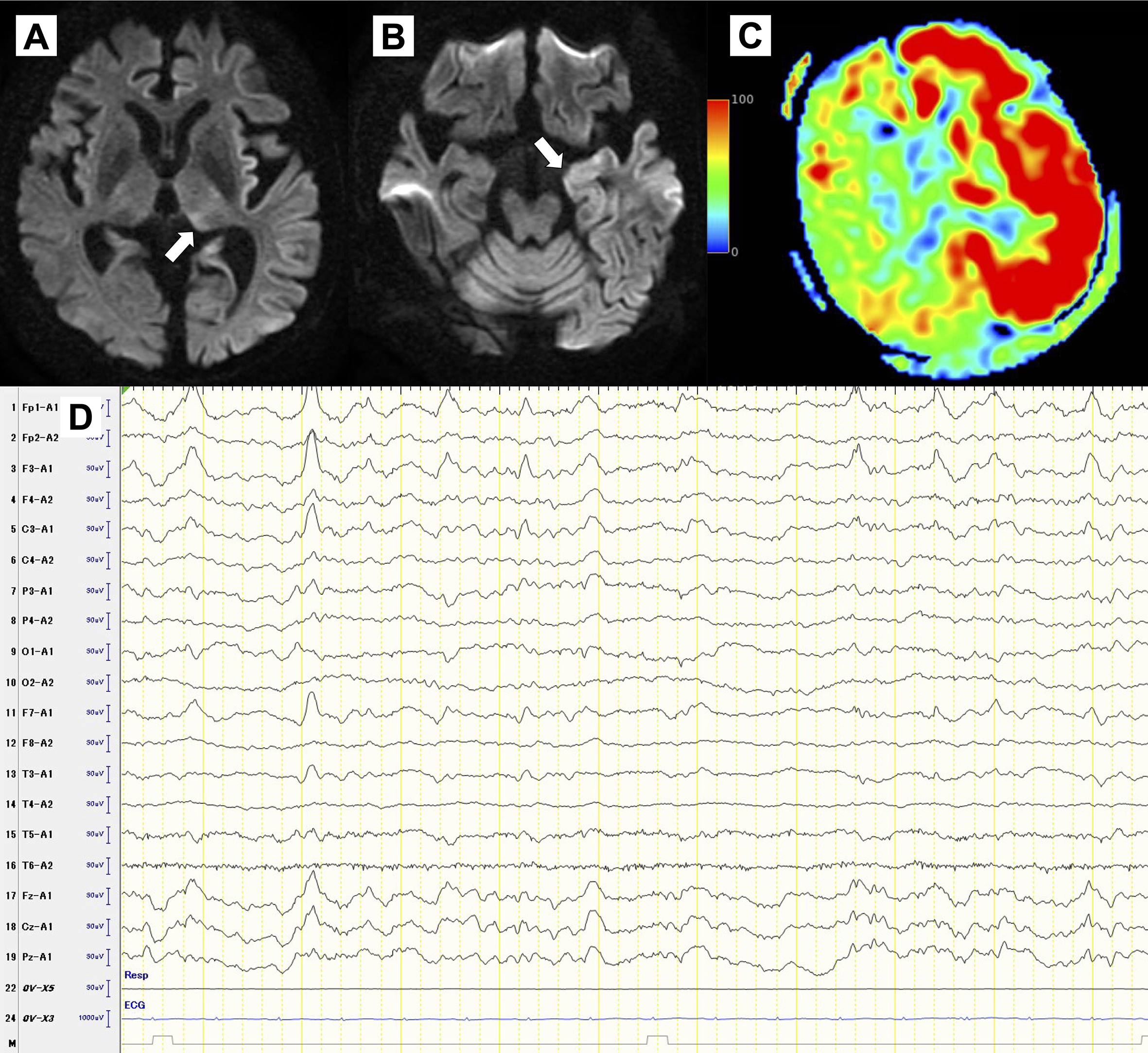
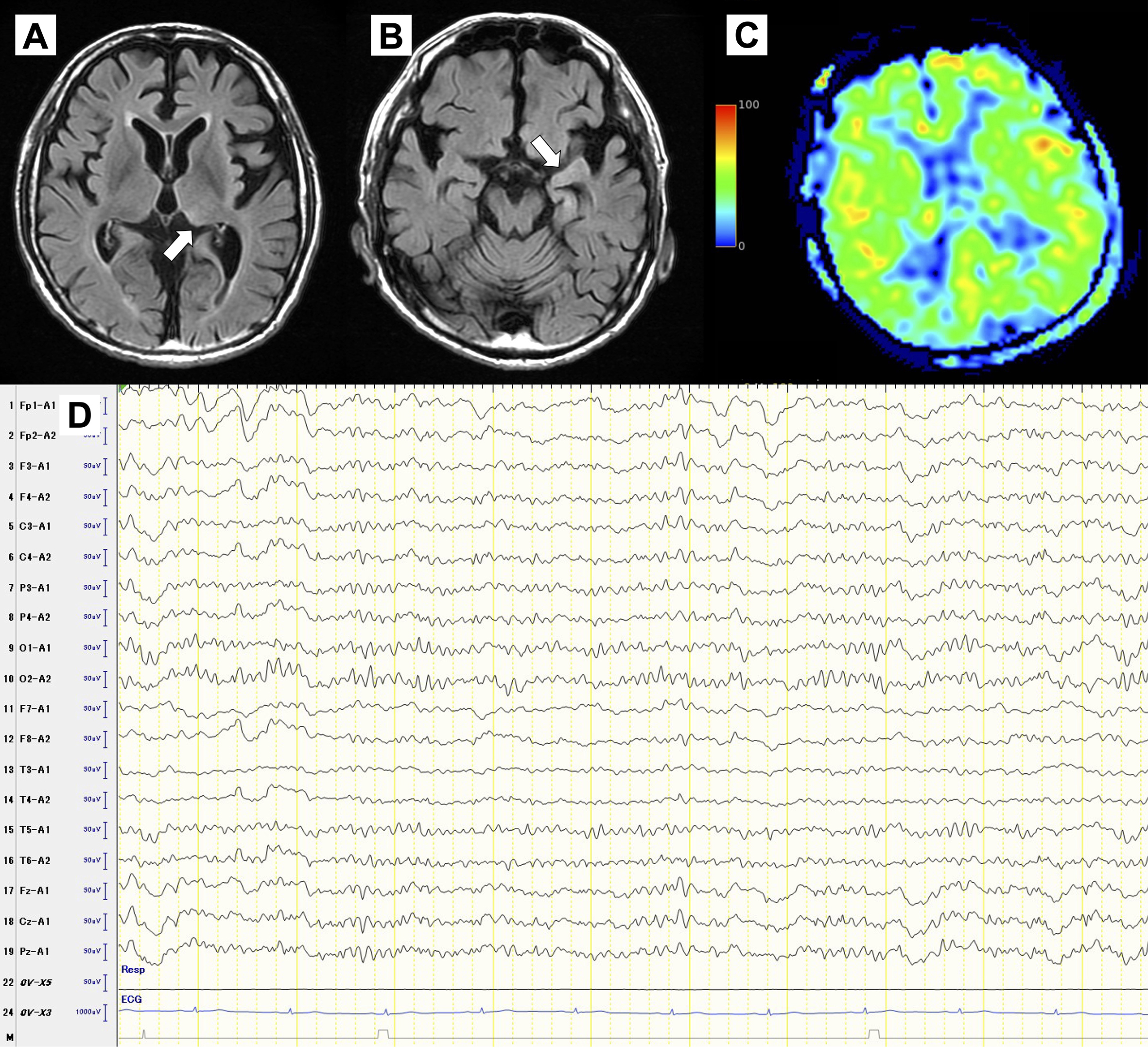
SESA syndrome is a rare condition in alcohol-dependent individuals (1). Unlike typical withdrawal, it often involves prolonged confusion and recurrent seizures, requiring long-term antiepileptic treatment (2), (3). MRI frequently shows transient cortical-subcortical T2-hyperintense areas with restricted diffusion, and EEG reveals focal abnormalities (2), (4). The diagnosis of SESA syndrome is crucial due to its distinct course and management.
None
The authors thank Yudai Imahayashi MD, Keita Majima MD, Asuka Mori MD, Masayoshi Kawaguchi MD, and Akari Saratani MD for their cooperation in patient care.
Rikuto Christopher Shinohara contributed to patient care, planning, conduct, and writing up the work. Shun Takayanagi, Yoichi Furutaka, and Shinya Watanabe provided critical revisions to the report. All authors reviewed and approved the final version.
Consent to publish the details of the present case was obtained from the patient.
Niedermeyer E, Freund G, Krumholz A. Subacute encephalopathy with seizures in alcoholics: a clinical-electroencephalographic study. Clin Electroencephalogr. 1981;12(3):113-29.
Fernández-Torre JL, Kaplan PW. Subacute encephalopathy with seizures in alcoholics syndrome: a subtype of nonconvulsive status epilepticus. Epilepsy Curr. 2019;19(2):77-82.
Fernández-Torre JL, Kaplan PW. Subacute encephalopathy with seizures in alcoholics (SESA syndrome) revisited. Seizure. 2014;23(5):393-6.
Drake-Pérez M, Marco de Lucas E, Lyo J, et al. Neuroimaging features in subacute encephalopathy with seizures in alcoholics (SESA syndrome). Seizure. 2016;40:102-7.