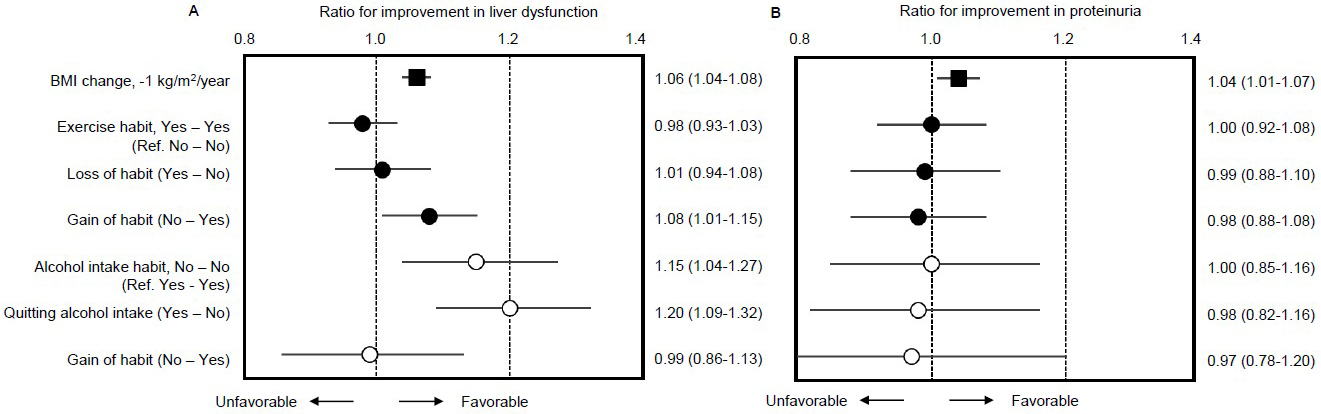
Figure 1. Inclusion and exclusion flow
The cohort study originated with 933,490 individuals from the general population who had participated in annual specific health checkups since 2008. Subjects in the first analysis were thus 591,671 individuals (58.8% women) for whom all of the data necessary for this study were available. Since the purpose of this study was to determine whether weight loss is associated with improvements in liver dysfunction and proteinuria, analysis was further limited to 36,256 obese individuals (body mass index ≥ 25 kg/m2 at baseline) with elevated levels of aspartate aminotransferase (AST) and/or alanine aminotransferase (ALT) (≥31 IU/L each) or positive proteinuria (+/− or more) in both the first and second years of the study. Of these final subjects, 27,615 had persistent liver dysfunction, 11,396 had persistent proteinuria, and 2,755 were duplicates. Outcomes for analysis were improvement of liver dysfunction and/or proteinuria during follow-up with a mean interval of 3.02 years from the second survey.
From: Weight Loss Improves Liver Dysfunction and Dipstick Proteinuria in Obesity: The Japan Specific Health Checkups Study
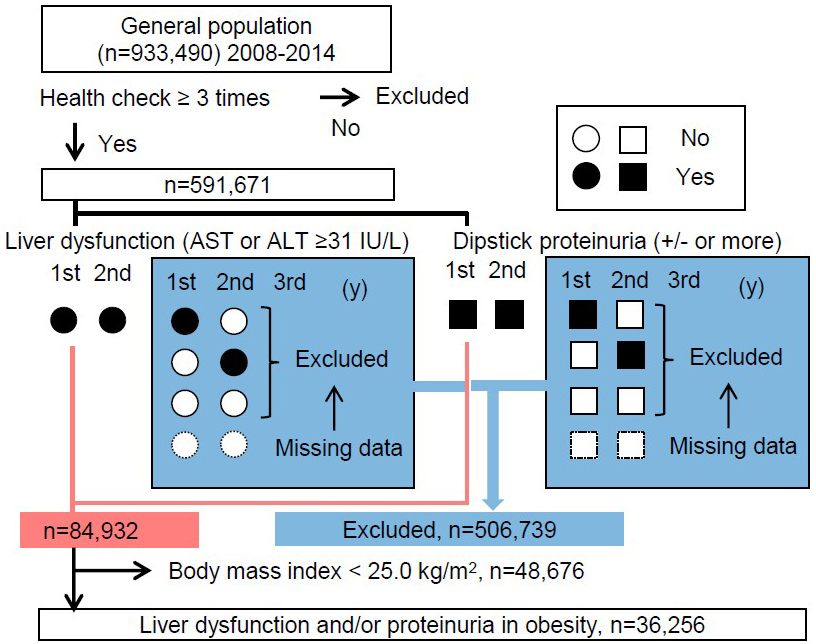
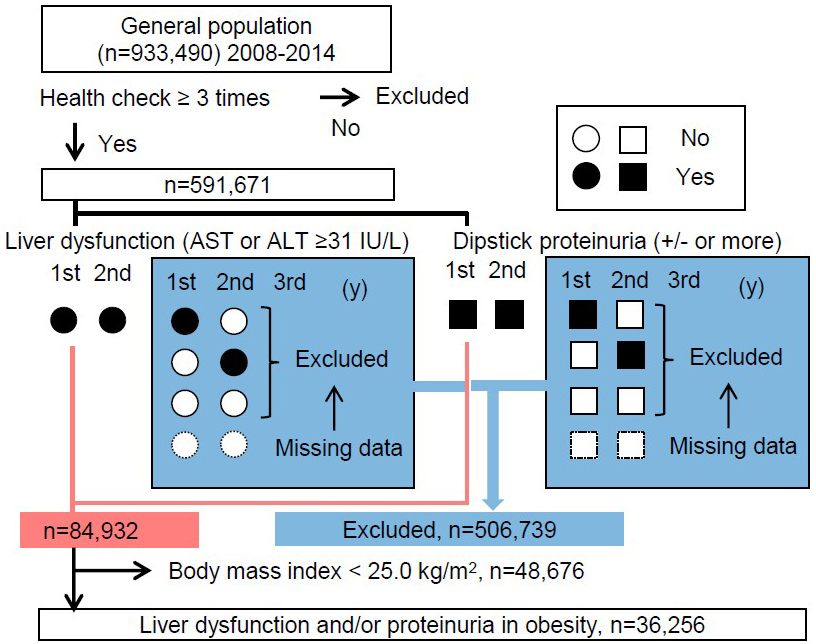
Figure 2. Distribution of body mass index with and without liver dysfunction and proteinuria
Among the 591,671 subjects just after the first exclusion based on the number of health checks, we examined the distribution and mean body mass index at baseline for 506,739 subjects to be excluded based on the absence of both liver dysfunction and proteinuria and for 84,932 subjects with liver dysfunction or proteinuria, respectively. Obesity is defined as body mass index ≥ 25 kg/m2 at baseline.
From: Weight Loss Improves Liver Dysfunction and Dipstick Proteinuria in Obesity: The Japan Specific Health Checkups Study
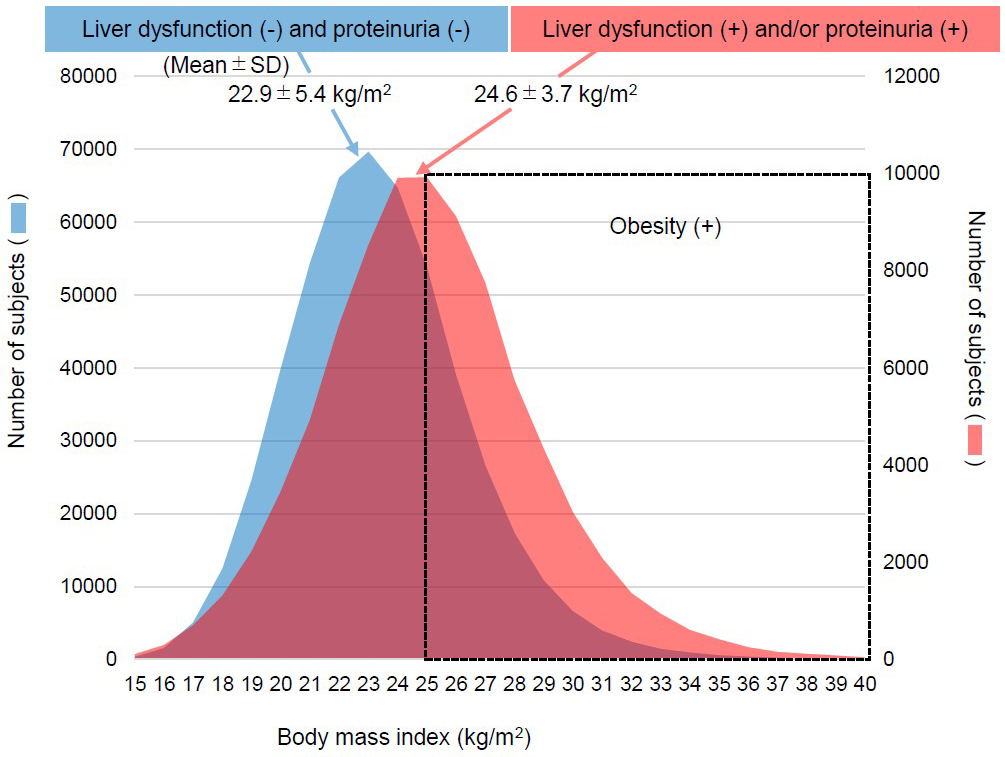
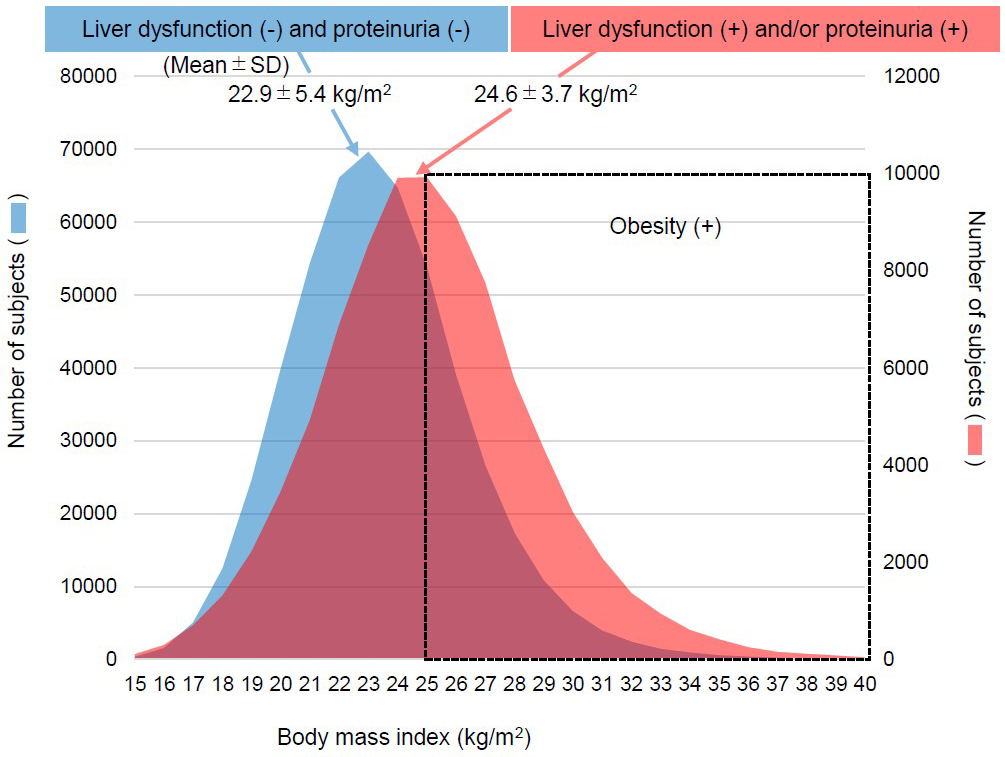
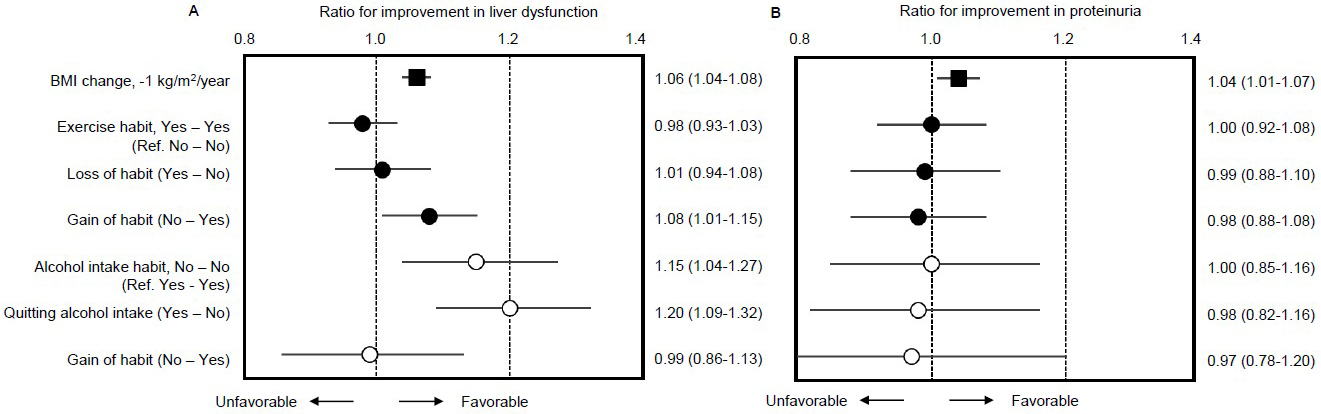
Figure 3. Multivariable-adjusted rates of improvement in liver dysfunction and proteinuria for the obese population with changes in body weight, exercise habit, and alcohol intake habit
Outcomes for analysis were the first improvement of liver dysfunction (A) and proteinuria (B) during follow-up and times to outcomes were assessed by Cox proportional hazards modeling with adjustment for factors described in the Methods section and shown in Table 2. Multivariable-adjusted hazard ratios and 95% confidence intervals for improvement are presented. The Specific Health Check questionnaire includes questions regarding lifestyle and habits using question items: “Light sweaty exercise for at least 30 minutes at least 2 days a week for at least 1 year” and “Current alcohol intake status.” We utilized baseline and subsequent information to define “Loss of habit” as a change from “yes” to “no” in participant answers and “gain of habit” as a change from “no” to “yes,” respectively.
From: Weight Loss Improves Liver Dysfunction and Dipstick Proteinuria in Obesity: The Japan Specific Health Checkups Study