Corresponding author: Yuichiro Haba, yhaba@juntendo.ac.jp
DOI: 10.31662/jmaj.2022-0128
Received: June 6, 2022
Accepted: November 24, 2022
Advance Publication: March 6, 2023
Published: April 14, 2023
Cite this article as:
Haba Y, Hashiguchi N. Adrenal Injury in Situs Inversus. JMA J. 2023;6(2):204-205.
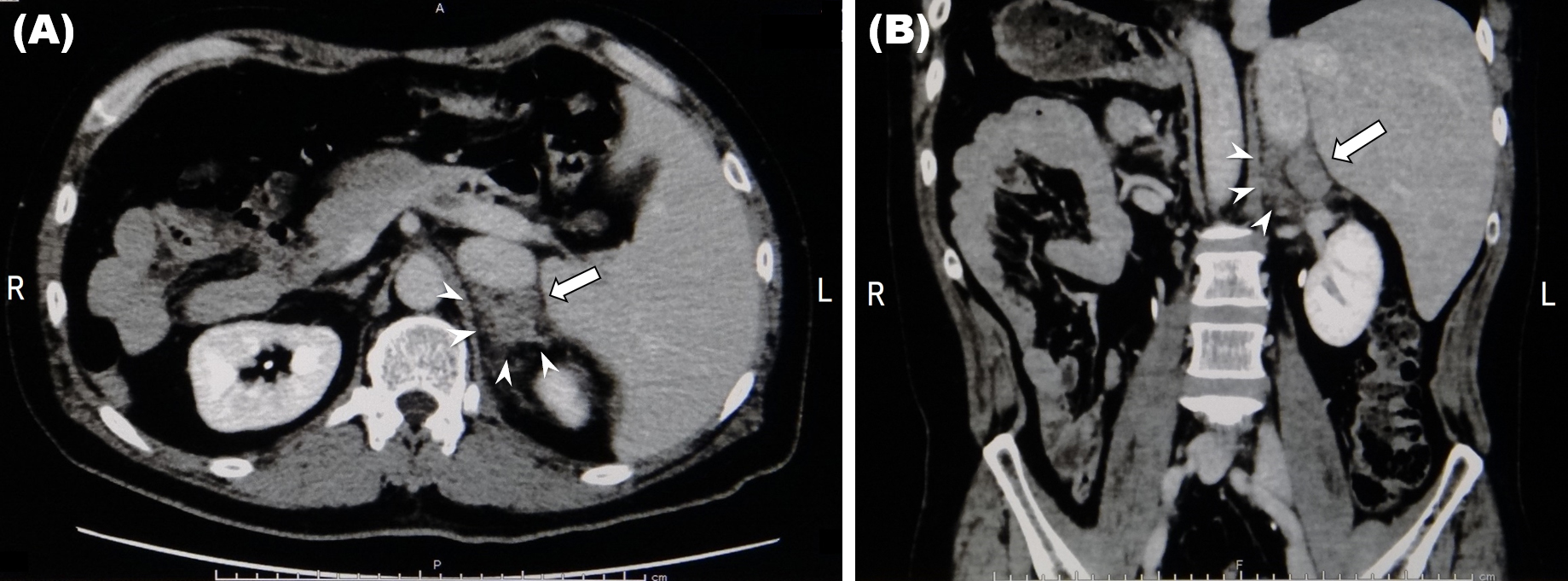
Key words: Blunt adrenal injury, Situs inversus, Primary care
A 43-year-old man presented to our primary care clinic with back pain and contusions following a motorcycle accident. Contrast-enhanced computed tomography revealed complete situs inversus, left upper rib fractures, left adrenal enlargement, and no evidence of extravasation or other organ damage. The left adrenal gland measured 3.1 cm along the major axis (Figure 1: arrow) and periadrenal fat stranding (Figure 1: arrowheads) was observed. Serum hormone tests ruled out neoplasia and the enlargement was attributed to trauma (1). Blunt trauma predominantly affects the right adrenal gland (1), (2), (3) owing to its proximity to vertebrae and drainage through the inferior vena cava (1), (4); the patient’s left-sided injury could be attributed to situs inversus. As with other reports (2), (3), (4), this case was nonoperative and successfully managed in the primary care setting. Our incidental discovery of situs inversus highlights one potentially disastrous consequence of estimating injury severity based on conventional anatomical features and eschewing diagnostic imaging.
None
All authors contributed to patient care. YH conceived the idea for the study and wrote the manuscript. NH contributed to the editing of the manuscript.
An IRB approval is not required because this is a case report.
Written informed consent was obtained from the patient for publication.
Sinelnikov AO, Abujudeh HH, Chan D, et al. CT manifestations of adrenal trauma: experience with 73 cases. Emerg Radiol. 2007;13(6):313-8.
Tanizaki S, Maeda S, Ishida H. Blunt adrenal gland injury: the impact of extra-abdominal injury. J Trauma Acute Care Surg. 2021;91(4):716-8.
Al-Thani H, El-Matbouly M, El-Menyar A, et al. Adrenal gland trauma: an observational descriptive analysis from a level 1-trauma center. J Emerg Trauma Shock. 2021;14(2):92-7.
de Camargo Galindo GF, Pagamisse OST, De Lima R, et al. Nonoperative treatment of a blunt adrenal gland trauma with blush: a case report. Trauma Case Rep. 2021;32:100454.