Corresponding author: Soichiro Saeki, sosaeki@hosp.ncgm.go.jp
DOI: 10.31662/jmaj.2022-0177
Received: September 24, 2022
Accepted: December 13, 2022
Advance Publication: March 13, 2023
Published: April 14, 2023
Cite this article as:
Saeki S, Kurosawa Y, Tomiyama K, Tomizawa R, Honda C, Minamitani K. Foreign Patients Visiting the Emergency Department: A Systematic Review of Studies in Japan. JMA J. 2023;6(2):95-103.
Background: As the number of non-native patients in Japan is increasing, emergency departments must provide proper care for international patients. However, no research has been conducted to determine the demographics of international patients that visit Japanese hospitals or the requirements to accept them. We aimed to organize the existing research and its patterns for foreign patients in Japan’s emergency departments and to identify the areas that require further research.
Methods: Systematic review of research articles indexed in MEDLINE and Ichushi-web (Japanese medical literature) was conducted. The search strategy was based on a previous study in Japanese, and the search was limited to manuscripts published from 2015.
Results: Nine publications that reported on the demographic characteristics of foreign patients who visited the emergency department were among the study’s 13 references. Injury diagnoses and the Asian population were both common. Dealing with overseas patients can be challenging due to linguistic barriers, cultural differences, and payment issues. However, studies describing the spoken language and the type of healthcare insurance used were lacking. Furthermore, neither the definition of “foreign patients” nor the distinction between short-term visitors and long-term residents were made in the majority of the research.
Conclusions: The demographic characteristics of patients differed depending on the location and facility, despite the fact that several characteristics of foreign patients in emergency departments appeared to be generalizable. The COVID-19 pandemic may modify the demographic characteristics of immigrants; thus, more research from a broad range of locations and medical facilities is still necessary.
Key words: migrant health, minority health, global health, non-national patients, foreigners
Migrant health is increasingly a worldwide issue in global health, even in high-income countries such as Japan (1). This covers the medical care for new immigrants or those who are descended from them, who may have varying histories from those of other local patients. The number of international tourists visiting Japan has climbed around six times since the start of the twenty-first century, despite a sharp decline in 2020 (2). In terms of foreign nationals living in Japan, 2.30% of the country’s population is made up of non-Japanese residents (2).
However, until recently, when the Japanese government started to implement measures to deal with the rising number of international tourists, the healthcare of patients without a Japanese identity was underappreciated (3). This includes developing practical guidance for patients with limited Japanese proficiency (LJP) (4) and accrediting certain medical facilities competent of delivering healthcare to foreign patients (5). Such measures were accelerated as Tokyo began investing in local prefectural governments to prepare for the Tokyo Olympic Games (3).
Nonetheless, many Japanese hospitals remain unprepared to deal with foreign patients. According to a national survey conducted by the Japan Hospital Association, approximately 95% of the hospitals in Japan answered that they were worried of linguistic issues if they were to deal with foreign patients (6). Previous studies on emergency departments in Japan have also highlighted the lack of linguistic assistance as a barrier in treating foreign patients (7), but studies to unravel further implications in the care for foreign patients have been lacking (8). This has been highlighted by the systematic review conducted by Tatsumi et al. (8) in 2016, when they found very few nationwide studies, as well as longitudinal or intervention studies. Furthermore, they did not find any studies in Japan that reported the characteristics of short-term foreign visitors (8).
To date, no study has been conducted to update the findings of Tatsumi et al. (8) As Japan has been eager to expand its ability to accept foreign patients, we projected that more research have been conducted in Japan in line with the growth in the trend to organize the environment for foreign patients.
Furthermore, the demographic features of foreign patients in Japan remain unknown. Identifying demographic features of foreign patients is important, as the medical requirements of foreign patients can be completely different from the locals (9), (10), (11), (12). Previous epidemiological studies have identified disparities between race and ethnicity in both acute (13), (14), (15) and chronic (16), (17), (18) medical conditions. Moreover, medical care for foreign patients requires detailed care focused on their linguistic, cultural, and religious backgrounds (19), (20), (21). Hence, understanding the current demographic features and the medical needs of foreign patients is of great necessity from the perspectives of public health and emergency medicine. Therefore, this study aims to identify major trends in Japanese studies to identify the characteristics of foreign patients in Japan and provide its key findings, as well as to indicate the research methodologies needed for studies that target foreign patients.
We conducted a systematic review focused on foreign patients in the emergency departments located in Japan. The review was organized according to the PRISMA statement (22).
Two databases, MEDLINE and Ichushi-web (Japanese medical literature), were searched on June 26, 2022. The search included keywords such as “foreigner,” “foreign patient,” “Japan,” and “emergency department” in English (MEDLINE) and Japanese (Ichushi-web). The search was limited to English and Japanese language manuscripts, published from January 1, 2015, to June 25, 2022, to cover for new literature that were published after the previous review (8).
All study designs that were (1) focused on foreign patients, (2) conducted in or reported from Japan, and (3) in the settings of pre-hospital emergencies or in the emergency departments were included for this study review. As the information to identify demographic features of foreign patients in emergency departments were focused on this study, case reports were excluded from the study.
Two authors independently reviewed every title and abstract of the identified manuscripts for inclusion and exclusion based on the eligibility criteria, completely blinded by each of the authors by using the Rayyan platform (23). The full-text papers were read to confirm the final inclusion decision. Disagreements were resolved upon discussion of the authors.
From the full-text articles presented, one author independently retrieved the data to report for this study. The following information was extracted from each study: publication year, study duration, study type, location of the study, study population, nationality of the patients, outcome, key findings, and how “foreign patients” were defined in each study. For the studies that reported the demographic features of the patients, the method of arrival, arrival time to the emergency department, nationality of the patients according to regions, diagnosis, and information regarding to the payment including unpaid medical expenses were obtained. No meta-analysis was conducted due to the nature of this study.
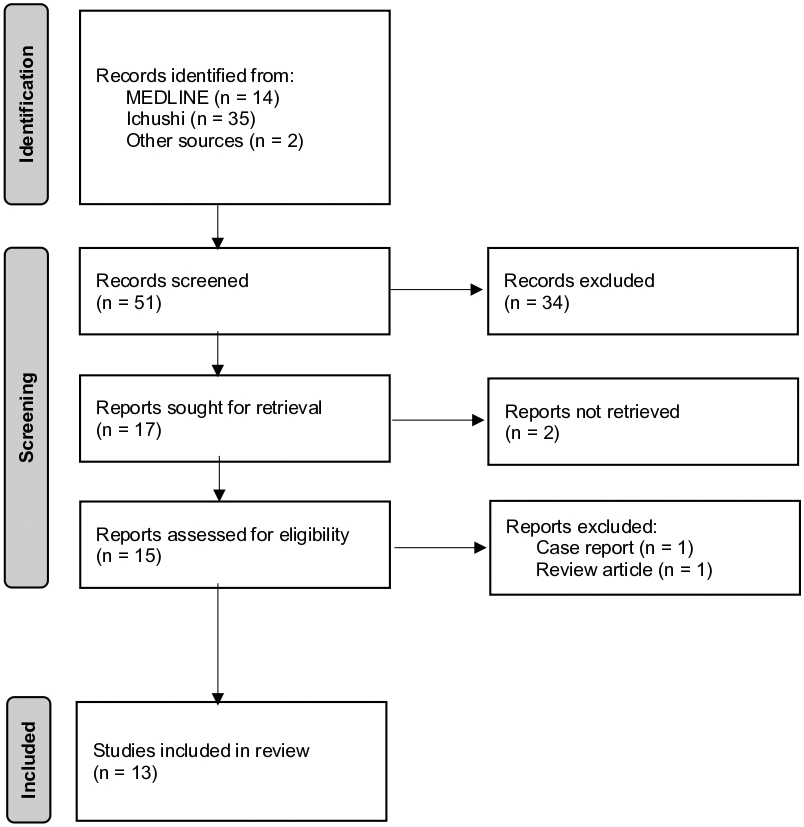
Figure 1 shows the inclusion and exclusion process according to the PRISMA statement. Forty-nine citations were found after searching the database, and two relevant citations not included in the databases were included. Upon initial title and abstract screening, 17 papers satisfied the inclusion criteria. Following a full-text review, two studies were excluded because one was categorized as a research article, while its content turned out to be a case report without study implications, and the other was the review by Tatsumi et al. (8) Thirteen manuscripts were evaluated qualitatively.
Of the 13 studies identified, 9 (24), (25), (26), (27), (28), (29), (30), (31), (32) were reported from hospitals reporting the demographic characteristics of foreign patients visiting the emergency department. Three studies were longitudinal studies (33), (34), (35) and one study was a quantitative study conducted targeting foreign patients in the emergency department (36). Regarding the years of publication, 2020 saw the most publications with four, followed by 2019 with three and 2018 and 2022 with two publications each. 2016 and 2017 had one publication each, and no studies were included in our review from 2021.
Table 1 shows the overview of the nine studies with the demographic characteristics of foreign patients visiting the emergency departments of Japan. All studies were conducted through a retrospective review of healthcare records, while one study reported results of the analysis from payment records also. The location of the hospitals of which the study was conducted ranged from the north to Hokkaido and Okinawa on the south. Two studies particularly focused on short-term visitors, but no study provided the specific information on how they defined their population or how they have been able to classify the patients as foreigners (Table 1-a).
Table 1-a. Overview of the Studies Describing Demographic Features of the Patients in Emergency Departments of Each Facility.
| Author | Year | Study duration | Study type | Location | Definition of “foreigners” | Population | |
|---|---|---|---|---|---|---|---|
| 24 | Takashina et al. | 2017 | January 2011―December 2015 | Retrospective review of medical records and accounting data | Kyoto | definition of “visitors” Provided | “Visitors” that visited or were referred to the emergency department |
| 25 | Taguchi et al | 2018 | April 2012―March 2016 | Retrospective review of medical records | Hokkaido | Not provided | Foreign patients |
| 26 | Oshita et al | 2019 | April 2015―March 2018 | Retrospective review of medical records | Yamanashi | Not provided | Foreign visitors |
| 27 | Kainuma et al | 2019 | April 2014―March 2019 | Retrospective review of medical records | Osaka | Not provided | Foreign patients |
| 28 | Suzaki et al. | 2019 | April―September 2017 | Retrospective review of medical records | Tokyo | Not provided | Foreign patients visiting the primary and secondary emergency department for the first time |
| 29 | Nakazawa et al. | 2020 | January 2014―December 2018 | Retrospective review of medical records | Okinawa | Not provided | Pregnant foreign patients in a single emergency department |
| 30 | Shimoyama et al. | 2020 | April 2015―March 2018 | Retrospective review of medical records | Tokyo | Not provided | Foreign patients transported to a tertiary care center |
| 31 | Aoki et al. | 2022 | April 2018―March 2020 | Retrospective review of medical records | Nagano | Not provided | Foreign patients transported to a tertiary care center |
| 32 | Ishii et al. | 2022 | January 2010―December 2019 | Retrospective review of medical records | Tokyo | Visual classification of patient names | Foreign patients transported to a tertiary care center |
| The year of publication, the duration when the study was conducted, each facility’s location (in prefecture), how each study defined foreigners, and the study population was derived from each study. | |||||||
All studies reported most of the patients being able to be discharged without requiring hospitalizations. However, the rate of patients arriving using ambulances or by walk-ins varied between studies. The arrival time also varied between each study (Table 1-b).
Table 1-b. Outcome, Severity, and the Time of Visit of Foreign Patients Defined in Each Study.
| Author | Year | Outcome | Transportation | Visits | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total patients | |||||||||||
| (included in the study) | Hospitalized | Deaths | Walk-in | Ambulance | Air transport | During daytime | During evenings | During nights | |||
| 24 | Takashina et al. | 2017 | 1059 | 46 (4%) | 1 (0%) | 744 (70%) | 314 (30%) | 0 | - | - | - |
| 25 | Taguchi et al | 2018 | 132 | - | - | - | 132 (100%) | - | 53 (40%) | 49 (37%) | 30 (33%) |
| 26 | Oshita et al | 2019 | 474 | - | 1 (0%) | 380 (80%) | 93 (20%) | 1 | 205 (43%) | 269 (57%) | - |
| 27 | Kainuma et al | 2019 | 198 | 13 (7%) | 3 (2%) | 56 (28%) | 142 (72%) | 0 | 142 (71%) | 56 (29%) | |
| 28 | Suzaki et al. | 2019 | 158 | 3 (2%) | 0 | 131 (83%) | 27 (17%) | 0 | 110 (70%) | 48 (30%) | |
| 29 | Nakazawa et al. | 2020 | 37 | 4 (11%) | 0 | - | - | - | 15 (41%) | 11 (30%) | 11 (30%) |
| 30 | Shimoyama et al. | 2020 | 87 | 55 (63%) | 25 (29%) | - | - | - | - | - | - |
| 31 | Aoki et al. | 2022 | 777 | 71 (9%) | 1 (0%) | 660 (85%) | 106 (14%) | 11 (1.4%) | 405 (52%) | 262 (34%) | 110 (14.2%) |
| 32 | Ishii et al. | 2022 | 325 | - | 27 (8.3%) | - | - | - | - | - | - |
| Hyphens are indicated where information was unretrievable. The percentages were calculated by the authors based on the number of total patients included in the study. Numbers indicated between several columns indicate the numbers as the sum of the indicated sections. | |||||||||||
Regarding the nationality of the patients, Asia was the most common population. However, the second largest population varied between the studies (Table 1-c). For most of the studies that did not focus on a single specific diagnosis, injury was the most common diagnosis for the study population. However, infectious and gastrointestinal diseases were also found to be common (Table 1-d).
Table 1-c. The Nationality of the Patients Reported in Each Study.
| Author | Year | Nationality | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Asia | Europe | Oceania | North America | Latin America | Others | Unknown | |||
| 24 | Takashina et al. | 2017 | 477 (45%) | 201 (19%) | 85 (8%) | 148 (14%) | 0 | 169 | 0 |
| 25 | Taguchi et al | 2018 | 84 (64%) | 3 (2%) | - | - | - | 0 | 25 |
| 26 | Oshita et al | 2019 | 369 (78%) | 42 (9%) | 24 (5%) | 34 (7%) | 1 (2%) | 0 | 4 |
| 27 | Kainuma et al | 2019 | 157 (79%) | 23 (12%) | 11 (6%) | 6 (3%) | 0 | 1 | 0 |
| 28 | Suzaki et al. | 2019 | 123 (78%) | 8 (5%) | 0 | 12 (8%) | 0 | 15 | 0 |
| 29 | Nakazawa et al. | 2020 | 32 (86%) | 0 | 2 (5%) | 2 (3%) | 1 (3%) | 0 | 0 |
| 30 | Shimoyama et al. | 2020 | 51 (74%) | 6 (9%) | 4 (6%) | 5 (7%) | 0 | 7 | 18 |
| 31 | Aoki et al. | 2022 | - | - | - | - | - | - | - |
| 32 | Ishii et al. | 2022 | - | - | - | - | - | - | - |
| Hyphens are indicated where information was unretrievable. The percentages were calculated by the authors based on the number of total patients included in the study. | |||||||||
Table 1-d. Diagnosis of Diseases Foreign Patients Presented within the Emergency Departments.
| Author | Year | Disease | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Infectious | Others/ | |||||||||||||
| Injury | Urology | OBGYN | Pediatrics | Neurology | GI | Cardiovascular | Respiratory | ENT | diseases | Toxicology | unspecified | |||
| 24 | Takashina et al. | 2017 | 295 (28%) | 106 (10%) | 21 (2%) | - | 21 (2%) | 164 (16%) | 32 (3%) | 202 (20%) | 32 (3%) | 169 | ||
| 25 | Taguchi et al | 2018 | 46 (35%) | 5 (4%) | - | - | - | 26 (20%) | - | 11 (8%) | - | - | 12 (9%) | 32 |
| 26 | Oshita et al | 2019 | 166 (35%) | 22 (5%) | 21 (4%) | 64 (14%) | 168 (35%) | - | - | - | - | - | - | 33 |
| 27 | Kainuma et al | 2019 | 72(36%) | 5 (2%) | - | - | 15(8%) | 32(16%) | 21(11%) | 8(4%) | 14 (7%) | - | - | 31 |
| 28 | Suzaki et al. | 2019 | 19 (12%) | 4 (3%) | 0 | 0 | 4 (3%) | 21 (13%) | 2 (1%) | 3 (2%) | 3 (2%) | 37 (23%) | 92 | |
| 29 | Nakazawa et al. | 2020 | - | - | 37 (100%) | - | - | - | - | - | - | - | - | - |
| 30 | Shimoyama et al. | 2020 | 16 (18%) | 4 (5%) | 37 (31%) | 3 (4%) | 12 (14%) | 24 | ||||||
| 31 | Aoki et al. | 2022 | 263 (33.9%) | 47 (6.0%) | - | - | - | 52 (67%) | - | 114 (14.7%) | - | 65 (8.4%) | - | 56 |
| 32 | Ishii et al. | 2022 | 73 (21.8%) | 0 | - | - | 14 (4.3%) | 56 (17.2%) | 73 (22.4%) | 16 (4.9%) | - | 17 (5.2%) | 28 (8.6%) | 48 |
| Injuries include self-harms and burns. Cerebrovascular diseases are included in either cardiovascular or neurology, depending on the study. Cardiopulmonary arrests (CPAs) are included in cardiovascular diseases. Hyphens are indicated where information was unretrievable. The percentages were calculated by the authors based on the number of total patients included in the study. OBGYN, obstetrics and gynecology; GI, gastrointestinal; ENT, otolaryngology |
||||||||||||||
Regarding the key findings in each study, linguistic issues posed as a major issue when dealing with foreign patients. In some hospitals, interpreting services were not commonly used, and communication difficulties were observed between the medical professionals and patients. Four studies mentioned about unpaid medical expenses by foreign patients (Table 1-e).
Table 1-e. Information on Payments by Foreign Patients and the Key Findings of Each Study.
| # | Author | Year | Payment | Key findings | |
|---|---|---|---|---|---|
| Outstanding | |||||
| Fee (JPY) | expenses | ||||
| 24 | Takashina et al. | 68,000/outpatient, | |||
| 745,000/inpatient, | Children accounted for 19.3% of the patients. | ||||
| 2017 | 174500/day/person | 1% of total | Many emergency transports were mild cases, and hospitalization was short at the average of 9.7 days. | ||
| 25 | Taguchi et al | 2018 | - | - | Cultural differences, linguistics, and religions posed as problems when dealing with foreign patients. |
| Dealing with foreign patients requires a comprehensive approach with medical and non-medical staff. | |||||
| 26 | Oshita et al | 2019 | - | - | There are differences in the needs of foreign patients between each location. |
| Whether patients understand translational devices are unknown. | |||||
| Some required hospitalizations but refused; whether this is due to linguistic problems remains difficult to evaluate. | |||||
| Passport documentations and death certificates for other countries posed as difficulties. | |||||
| 27 | Kainuma et al | 2019 | 108,000 ± 453,340 | 6 (3%) | Communication was mainly possible with the usage of interpreting device. |
| Unpaid medical expenses became a problem although many tourists had travel insurance. | |||||
| 28 | Suzaki et al. | 2019 | - | 3 (2%) | Infectious diseases, which were of common diseases, were also common among foreign patients. |
| Primary and secondary emergency departments also had a high number of injuries. | |||||
| Some cases included several refusals of other medical facilities. | |||||
| Eight percent of patients with residency in Japan did not have a national healthcare insurance. | |||||
| 29 | Nakazawa et al. | 2020 | - | - | Difficulty was found in retrieving information on the gynecological status of patients from other countries. |
| Arrival in ambulances was common among foreign patients than Japanese patients. | |||||
| 30 | Shimoyama et al. | 2020 | 1,0009,735/case | 13 (15%) | Forty-two percent of the patients were covered with a Japanese public healthcare insurance. |
| Fifty-four percent of the cases required linguistic assistance, but professional interpreting was provided in only one case. | |||||
| Difficulty was found in gaining informed consent and planning international transfers. | |||||
| 31 | Aoki et al. | 2022 | - | - | Language used when treating the patients was associated with length of stay in the emergency department. |
| 32 | Ishii et al. | 2022 | - | - | Anaphylaxis, burn, and infectious disease diagnoses were more common among non-Japanese patients. |
| No statistical significance was found in mortality rates or mean lengths of stay with stratification on language or disorientation of the CNS. | |||||
| Hyphens are indicated where information was unretrievable. The percentages were provided in each study. Key findings were derived quantitatively. JPY, Japanese yen |
|||||
Table 2 summarizes the quantitative and longitudinal studies that focused on foreign patients who visited the emergency room of Japanese medical facilities. The three longitudinal studies were conducted in Osaka, while the qualitative study was conducted in a hospital in Tokyo.
Table 2. Overview of the Longitudinal and Qualitative Studies in the Review.
| # | Author | Year | Duration | Study type | Location | Population | Definition of “foreigners” | Outcome | Key findings |
|---|---|---|---|---|---|---|---|---|---|
| 33 | Katayama et al | 2016 | Jan–Dec 2013 | Retrospective study of EMS records | Osaka City | Patients using ambulances in Osaka City | Not defined | Characteristics of patients who experienced difficulty in hospital acceptance at the scene by emergency medical service personnel | Being a foreign patient was associated with difficulty in hospital acceptance at scene |
| Difficulty may have occurred due to lack of multilingual staff in hospitals of Osaka | |||||||||
| 34 | Kishi et al. | 2018 | Jan 10–July 31, 2018 | Survey | Osaka Pref. | Hospitals with emergency departments in Osaka Prefecture | Not defined | Concerns when treating a foreign patient | Seventy-one percent of the facilities had difficulty as they had no interpreter. Thirty-eight percent of the hospitals experienced outstanding accounts. |
| 35 | Kishi et al. | 2020 | Jan 10–Dec 28, 2018 | Survey | Osaka Pref. | Hospitals with emergency departments in Osaka Prefecture | Not defined | Concerns when treating a foreign patient | Seventy-two percent of the facilities had difficulty as they had no interpreter. Thirty-six percent of the hospitals experienced outstanding accounts. Issues regarding the patients’ perception toward medicine, religion, diet, and patient transfers arose as new problems in hospitals. |
| 36 | Beppu et al. | 2020 | 2017.7–2018.1 | Interview | Tokyo | Foreign patients over 20 years old that did not speak Japanese in an emergency department | Not provided | Pain, cultural difficulties, communication difficulties, worries on reoccurrence of the symptoms, and worries on payment were noted as difficulties. | Physical difficulties are more critical in emergency departments compared to the Japanese. Difficulties change during the clinical course. |
| The year of publication, the duration when the study was conducted, each facility’s location, how each study defined foreigners, the study population, outcomes, and key findings focused on foreign patients were derived from each study. | |||||||||
Of the longitudinal studies, one study was not necessarily focused on foreign patients. Rather, being a foreign patient was one of the key outcomes in the study mainly focused on the general population of Osaka City. The other two studies were surveys conducted among hospitals in Osaka Prefecture and highlighted the difficulties without interpreters and cases with outstanding accounts when dealing with foreign patients.
The qualitative study was an interview focused on the difficulties foreign patients face in the emergency department. This study also identified that the difficulties foreign patients experience change during over the clinical course.
In this review, we have summarized the studies conducted in Japanese emergency departments that focus on foreign patients. To date, our study is the first to review the studies that have been published near the Tokyo Olympic Games, which had been one of the key events that Japan focused on when organizing the environment to accept foreign patients (3).
Compared to the previous manuscript published in 2016 (8), three study trends arose. Firstly, the number of publications per year has increased. Secondly, reports that included information regarding short-term visitors were included. Thirdly, more studies reported the demographic features of foreign patients. These will all contribute to further understandings of non-national patients that visit the emergency department.
Many studies focused on the demographic features of foreign patients. Many of the patients were from Asian countries, and many studies reported injuries to be common among foreign patients. As Japan is an island nation located in Asia, Asian patients being common is a reasonable result. Injuries are also reported to be common among short-term visitors in other countries (37), and this may be a trend that can be generalized for travel medicine. In addition, many foreign patients were discharged after receiving treatment.
Studies also highlighted the necessity for linguistic assistance. Linguistic assistance could aid communication to inform patients in detail about their health status (38), (39), and inadequate communication could have led to an excess amount of discharge for foreign patients. Furthermore, as foreign patients are more likely to experience financial and linguistic difficulties than local patients (40), a lack of effective communication may have increased the risk of outstanding accounts, when medical staff could not have provided information regarding the medical expenses necessary for treatment. As studies in this review have highlighted, providing linguistic assistance and financial support to indemnify for the outstanding accounts from foreign patients would be necessary when promoting Japanese hospitals to accept foreign patients in the emergency departments.
From the patient’s perspective, foreign patients are likely to experience unique difficulties when visiting Japanese emergency departments. As they receive treatment, they are likely to face cultural difficulties in addition to linguistic barriers, as well as to anxiety from the differences in the medical system compared to their homeland. Healthcare professionals should bear this in mind and try to communicate as effectively as possible using the greatest tools at their disposal, which may include medical interpreting services or other interpreting technologies.
Although the number of studies increased during the recent years, further studies are still necessary to address the issues in migrant health in emergency departments. From this review, several factors that should be included in further studies, as well as future research questions, have emerged.
Firstly, criteria to report when discussing the demographic features of foreign patients must be clarified. One, how the study population were defined should be described more in detail. Although several studies have stated the definition of the “foreign patients” included in the study, no study reported the objective criteria that were used to define the patients. To fully define patients as foreigners, recording identifications may become necessary (12). Two, whether the patients were temporary visitors or residents should be disclosed. Some manuscripts reported demographic information of the patients only focused on visitors, but they did not state how they identified patients to be visitors. This would require recording the visa types or other documentations also (12), (41), which can also be troublesome for hospitals (42). Three, the type of insurance should also be reported. This would also aid grouping the patients as visitors or residents (12) and also generate a better idea on how to deal with outstanding expenses. Most hospitals keep record of the public healthcare insurance, and this data may be simpler to report than other official documentations. Four, the languages of the patients should be reported. Most studies reported linguistic difficulties, but the linguistics that was difficult to communicate with remains unclear.
Secondly, potential research questions arose from this study. One, studies that report the outcomes comparing the Japanese, foreign visitors and foreign residents would be necessary. It is thought that the medical demands of foreign visitors and residents are different (12), but the current studies have not been able to clearly identify such differences. Two, studies focused on linguistic communication would still be necessary. Compared to previous studies, more studies are reporting the use of linguistic assistance such as medical interpreting, but its advantages in the emergency departments in Japan remain unclear. Three, further studies reporting the demographics of overseas patients would be required. The novel coronavirus disease (COVID-19) pandemic has resulted in a dramatic decrease in the number of foreign visitors to Japan (2), and the demographic features of the patients may change. In addition, our study revealed that the demographic features of patients are different among regions, and thus, more studies from various regions would still be necessary.
This study has several limitations. Firstly, although we conducted the search for publications comprehensively including English and Japanese databases, publication bias is to be noted. We believe that many of the medical facilities in Japan that accept foreign patients do not routinely record these experiences, and the number of foreign patients in each facility may be few. The number of publications in this field may be decreased as a result of healthcare staff in such facilities failing to recognize their data as being important enough to publish. Secondly, the generalizability of this study should be addressed. Many of the facilities included in the study were accredited to accept foreign patients or had linguistic resources available. Data of such facilities may not be transferable to other facilities with fewer resources. Furthermore, longitudinal studies included in this manuscript were restricted to studies conducted in Osaka, which may not accurately represent the situations in other regions of Japan.
This review provided an overview of the recent studies conducted in Japanese emergency department focused on foreign patients. As the number of studies increased until the COVID-19 pandemic, the number and variety of studies remain few. Further studies examining various features, especially the outcomes, would still be necessary. As the demographic features of foreign patients may change due to travel restrictions from during and after the COVID-19 pandemic, we await further studies to be conducted.
None
Conceptualization, S.S.; methodology, S.S.; software, S.S.; validation, Y.K.; formal analysis, S.S.; investigation, S.S. and Y.K.; writing―original draft preparation, S.S.; writing―review and editing, Y.K., K.T., R.T., C.H., and K.M.; visualization, S.S.; supervision, K.T., R.T., C.H., and K.M. All authors have read and agreed to the published version of the manuscript.
Not applicable
Global health: time for radical change? Lancet. 2020;396:1129.
Immigration Services Agency of Japan. 2021 - Immigration control and residency management. [Internet] 2022 [cited 2022 Dec 1]. Available from: hhttps://www.moj.go.jp/isa/policies/policies/03_00015.html.
Saeki S, Minamitani K. The true legacy of the 2020 Tokyo Olympic Games to the 2025 World Expo: a step forward to racial equity in the Japanese healthcare system. J Int Health. 2021;36:151-2.
Nakamura Y. Importance and necessity of medical interpreters from the perspective of the current situation in Japan. Health Care. 2020;62:580-5.
Hinohara Y. Globalisation of the healthcare services sector: employing foreign physicians in national strategic special zones in Japan. Atlantis Press; 2019. p. 9-17.
Japan Hospital. Association. Report: Survey on the current status of international expansion of medical care. [Internet] 2015. [cited 2022 Dec 1]. Available from: https://www.hospital.or.jp/pdf/06_20151028_01.pdf.
Osegawa M, Morio H, Nomoto K, et al. Present medical practice and problems in emergency disease in foreign travelers requiring hospital admission. Nihon Kyukyu Igakukai Zasshi. 2002;13(11):703-10. Japanese.
Tatsumi Y, Sasaki-Otomaru A, Kanoya Y. The actual situation and issues of emergency medical services for foreigners staying in Japan extracted by systematic review. J Jpn Health Med Assoc. 2016;25:91-7.
Nielsen SS, Krasnik A. Poorer self-perceived health among migrants and ethnic minorities versus the majority population in Europe: a systematic review. Int J Public Health. 2010;55(5):357-71.
Moullan Y, Jusot F. Why is the ‘healthy immigrant effect’ different between European countries? Eur J Public Health. 2014;24(Suppl 1):80-6.
Helgesson M, Johansson B, Nordquist T, et al. Healthy migrant effect in the Swedish context: a register-based, longitudinal cohort study. BMJ Open. 2019;9(3):e026972.
Saeki S, Minamitani K, Muraki I, et al. Defining foreign patients as ‘visitors’ and ‘residents’ in Japanese medical facilities: difficulties in the collection of adequate data. J Epidemiol. 2022;32(2):112-3.
Luck AN, Preston SH, Elo IT, et al. The unequal burden of the Covid-19 pandemic: capturing racial/ethnic disparities in US cause-specific mortality. SSM Popul Health. 2022;17:101012.
Chavez S, Huebinger R, Chan HK, et al. Racial/ethnic and gender disparities of the impact of the COVID-19 pandemic in out-of-hospital cardiac arrest (OHCA) in Texas. Resuscitation. 2022;179:29-35.
Rodriguez F, Solomon N, De Lemos JA, et al. Racial and ethnic differences in presentation and outcomes for patients hospitalized with COVID-19: findings from the American Heart Association’s COVID-19 cardiovascular disease registry. Circulation. 2021;143(24):2332-42.
Saeki S, Szabo H, Tomizawa R, et al. Lobular difference in heritability of brain atrophy among elderly Japanese: a twin study. Medicina. 2022;58(9):1250.
Piroska M, Tarnoki DL, Szabo H, et al. Strong genetic effects on bone mineral density in multiple locations with two different techniques: results from a cross-sectional twin study. Medicina. 2021;57(3):248.
Saeki S, Yamamoto K, Tomizawa R, et al. Utilizing graphical analysis of chest radiographs for primary screening of osteoporosis. Medicina. 2022;58(12):1765.
Okamoto M, Matsuda Y, Foronda CL. Healthcare needs and experiences of foreign residents in Japan by language fluency. Public Health Nurs. 2022;39(1):103-15.
Kondo A, Kambayashi C, Koizumi M, et al. Factors related to difficulty in caring for foreign patients among nurses in Japanese hospitals. J Int Health. 2021;36:39-47.
Fortier JP. Improving healthcare for foreigners in Japan: lessons from Japan and abroad. J Jpn Acad Nurs Eval. 2015;5:81-7.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178-89.
Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Takashina K, Matoba H, Takegami T. Status and issues of foreign visitors in our hospital. The Journal of the Kyoto Medical Association. 2017;64:73-8.
Taguchi D, Makise H, Ishida H. A study on foreign patients presenting with abdominal symptoms. Nihon Fukubu Kyukyu Igakkai Zasshi. 2018;38:483-8.
Oshita Y, Yagi T, Hirabayashi K, et al. Survey of emergency hospital visits by foreign tourists in Japan. J Showa Univ Soc. 2020;79:752-6.
Kainuma M, Yasunaga Y, Asano T, et al. Current status of foreign patients visiting our hospital for emergency care. Jpn J Hosp Gen Med. 2019;15:534-9.
Suzaki M, Miyauchi M, Ohara T, et al. Current situation and issues of foreign patient care in the ER. Jpn J Hosp Gen Med. 2019;15:38-42.
Nakazawa T, Ohata T, Ishiduka T, et al. Obstetrical emergencies of foreign tourists in Okinawa. Journal of Japan Society of Perinatal and Neonatal Medicine. 2020;56:96-100.
Shimoyama K, Azuma K, Oda J. Analysis of severe foreign patients transported to our emergency department. J Jpn Soc Emerg Med. 2020;23:19-26.
Aoki Y, Kumazaki H, Terakawa I, et al. Factors associated with emergency department length of stay of foreign patients visiting a regional core hospital in Japan. Acute Med Surg. 2022;9(1):e758.
Ishii E, Nawa N, Matsui H, et al. Comparison of disease patterns and outcomes between non-Japanese and Japanese patients at a single tertiary emergency care center in Japan. J Epidemiol. 2022;32(2):80-8.
Katayama Y, Kitamura T, Kiyohara K, et al. Factors associated with the difficulty in hospital acceptance at the scene by emergency medical service personnel: a population-based study in Osaka City, Japan. BMJ Open. 2016;6(10):e013849.
Kishi M, Ihara I, Kusano T, et al. Questionnaire on the actual state of emergency medical care for foreign visitors in Osaka Prefecture. Osaka Kyukyu. 2018:9-14.
Kishi M, Kusano T, Ihara I, et al. Questionnaire on the actual state of emergency medical care for foreign visitors in Osaka Prefecture - an update. Osaka Kyukyu. 2020;3-7.
Beppu K, Kiuchi M, Yorozu H, et al. Difficulties encountered by foreign patients who was emergency transported and requiring emergency hospitalization. Journal of the Japanese Society of Travel and Health. 2020;14:6-11.
Mauritz W, Brazinova A, Majdan M, et al. Hospital admissions for traumatic brain injury of Austrian residents vs. of visitors to Austria. Brain Inj. 2014;28(10):1295-300.
Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255-99.
Lindholm M, Hargraves JL, Ferguson WJ, et al. Professional language interpretation and inpatient length of stay and readmission rates. J Gen Intern Med. 2012;27(10):1294-9.
Saeki S, Taniguchi H, Arahori H, et al. An international aircraft transport of a neonate from Georgia to Japan. Cureus. 2022;14(9):e28952.
Saeki S, Tomiyama K. Foreign patients in emergency departments of Japanese medical facilities. Acute Med Surg. 2022;9(1):e781.
Saeki S. Impact of the ‘Amendments to the Act of the Protection of Personal Information’ to global health research conducted in Japanese Medical Facilities. J Epidemiol. 2022;32(9):438.