Corresponding author: Yosuke Ono, onoyousuke1979@yahoo.co.jp
DOI: 10.31662/jmaj.2023-0057
Received: April 12, 2023
Accepted: June 1, 2023
Advance Publication: September 27, 2023
Published: October 16, 2023
Cite this article as:
Kobayashi T, Fujita N, Sekizawa A, Ono Y. Unilateral Leg Edema and Hydronephrosis in IgG4-Related Retroperitoneal Fibrosis. JMA J. 2023;6(4):541-542.
Key words: IgG4-related retroperitoneal fibrosis, hydronephrosis, leg edema
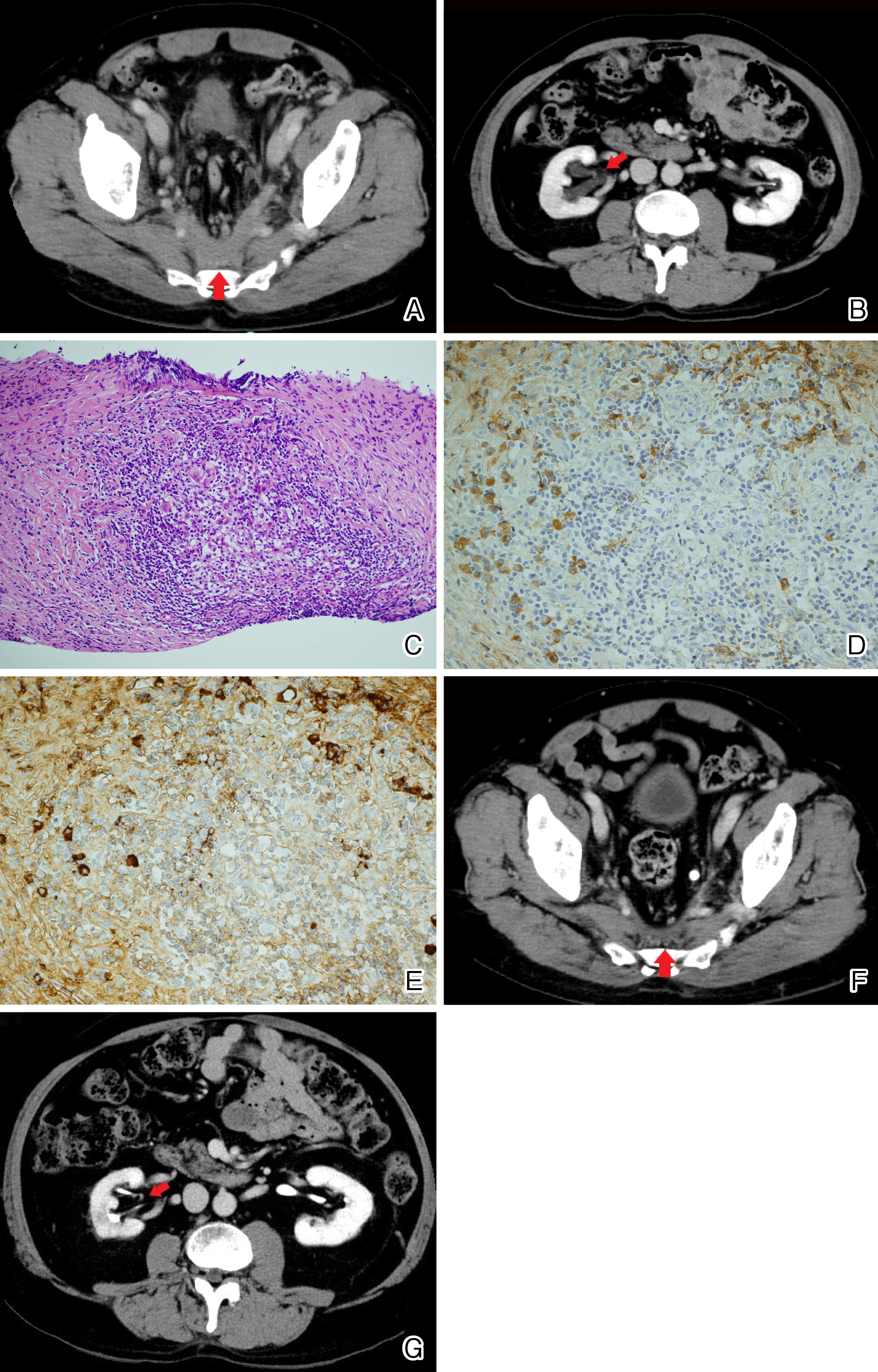
A 69-year-old man presented with a 2-month history of left leg edema. A contrast-enhanced computed tomography (CT) scan showed a mass occupying the caudal retroperitoneal area surrounding the pelvic arteries and veins (Figure 1A, red arrow). Laboratory findings demonstrated a high serum IgG4 concentration of 304 mg/dL (reference range, 11-121 mg/dL) greater than 135 mg/dL. Although the leg edema subsequently disappeared, the enlarging mass suppressed the right ureter, causing right-side hydronephrosis (Figure 1B, red arrow). His worsening renal dysfunction warranted ureteral stenting; however, he refused the procedure. A specimen from the retroperitoneal mass obtained using CT-guided biopsy revealed lymphoplasmacytic infiltration with storiform fibrosis, the number of IgG4-positive plasma cells greater than 10 per high powered field, and the ratio of IgG4-positive plasma cells/IgG-positive cells greater than 40% (Figure 1C, 1D and Figure 1E), leading to a definitive diagnosis of IgG4-related disease (1), (2). After 2 months of oral prednisolone and azathioprine treatment, the mass shrank and hydronephrosis subsequently improved (Figure 1F and 1G, red arrow). This case highlights the importance of evaluating the anatomical compression of veins and ureters by a retroperitoneal mass. Invasive ureteral stenting for hydronephrosis can be avoided if immunosuppressive treatment is effective for IgG4-related retroperitoneal fibrosis. Shared decision-making through patient-centered care was useful even in situations where the progressive organ dysfunction requiring surgical intervention was inevitable.
None
This work was supported by the Japan Medical Education Foundation (https://www.jmef.or.jp/).
TK wrote the first draft of the manuscript and NF, AS, and YO revised the manuscript. Furthermore, TK and NF contributed to patient care and YO organized the manuscript.
The patient provided written informed consent for the publication of the manuscript and clinical images.
This study did not require IRB approval.
Umehara H, Okazaki K, Kawa S, et al. The 2020 revised comprehensive diagnostic (RCD) criteria for IgG4-RD. Mod Rheumatol. 2021;31(3):529-33.
Kawano M, Saeki T, Nakashima H. IgG4-related kidney disease and retroperitoneal fibrosis: an update. Mod Rheumatol. 2019;29(2):231-9.