Corresponding author: Daichi Motomura, r2051md@jichi.ac.jp
DOI: 10.31662/jmaj.2024-0345
Received: November 15, 2024
Accepted: November 29, 2024
Advance Publication: January 31, 2025
Published: April 28, 2025
Cite this article as:
Motomura D, Takanosu T. Cerebral Fat Embolism Syndrome. JMA J. 2025;8(2):602-605.
Key words: fat embolism, consciousness, fracture
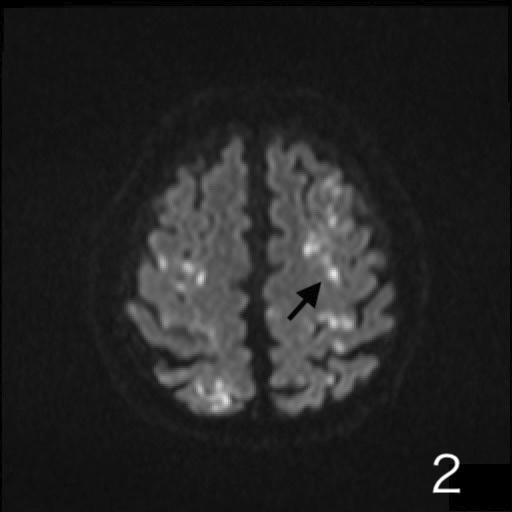
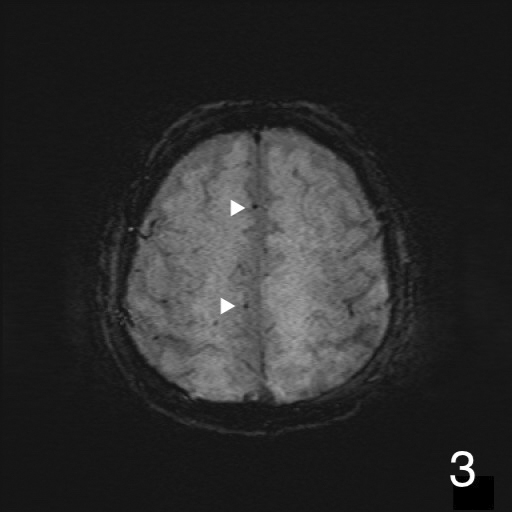
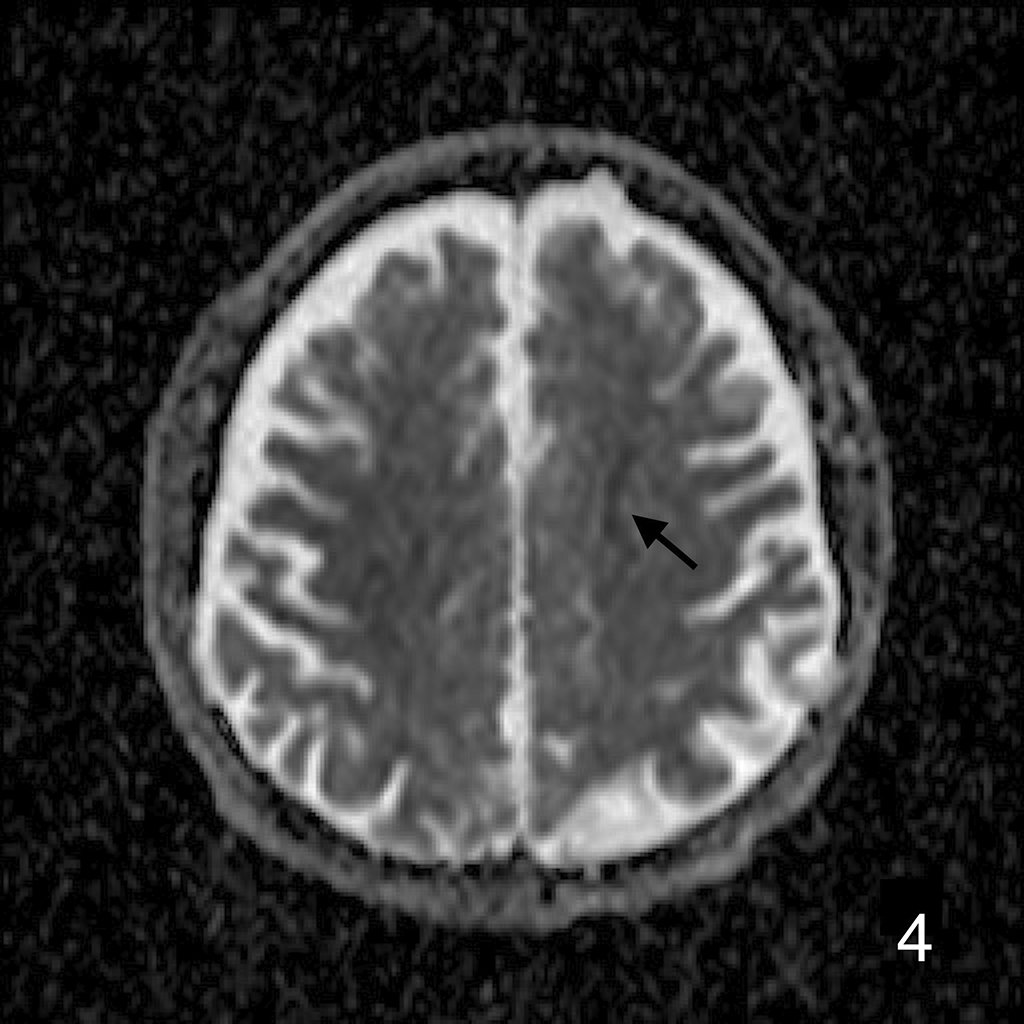
A 72-year-old man was presented to our hospital after falling. He was alert upon arrival, and diagnostic tests confirmed a fracture on the left femoral shaft (Figure 1). He was admitted to our hospital. On the 2nd day of admission, he suddenly developed altered consciousness and hypotension. He showed no signs of respiratory failure or skin manifestation. No intracranial abnormalities were identified in computed tomography performed on the same day. On the 3rd day of admission, the patient’s condition worsened, progressing to a comatose state. Brain magnetic resonance imaging revealed a star field pattern and diffuse microhemorrhages (Figure 2, 3, 4 and 5). Therefore, the patient was diagnosed with fat embolism syndrome. Owing to hemodynamic instability, internal fixation of the femoral shaft fracture was performed on the 6th day of admission. His level of consciousness gradually improved, and he was transferred to a rehabilitation facility.
None
Daichi Motomura wrote the first draft of the manuscript, and all authors commented on the previous versions of the manuscript. All the authors have read and approved the final version of the manuscript.
Informed consent was obtained by the opt-out method prescribed by the hospital.