Corresponding author: Daisuke Taniyama, daisuketaniyama@gmail.com
DOI: 10.31662/jmaj.2019-0045
Received: July 10, 2019
Accepted: August 15, 2019
Advance Publication: October 10, 2019
Published: January 15, 2020
Cite this article as:
Taniyama D, Maruki T, Sakai T. Relapsing Polychondritis. JMA J. 2020;3(1):75-77.
Key words: relapsing polychondritis, bronchoscopy, airway obstruction
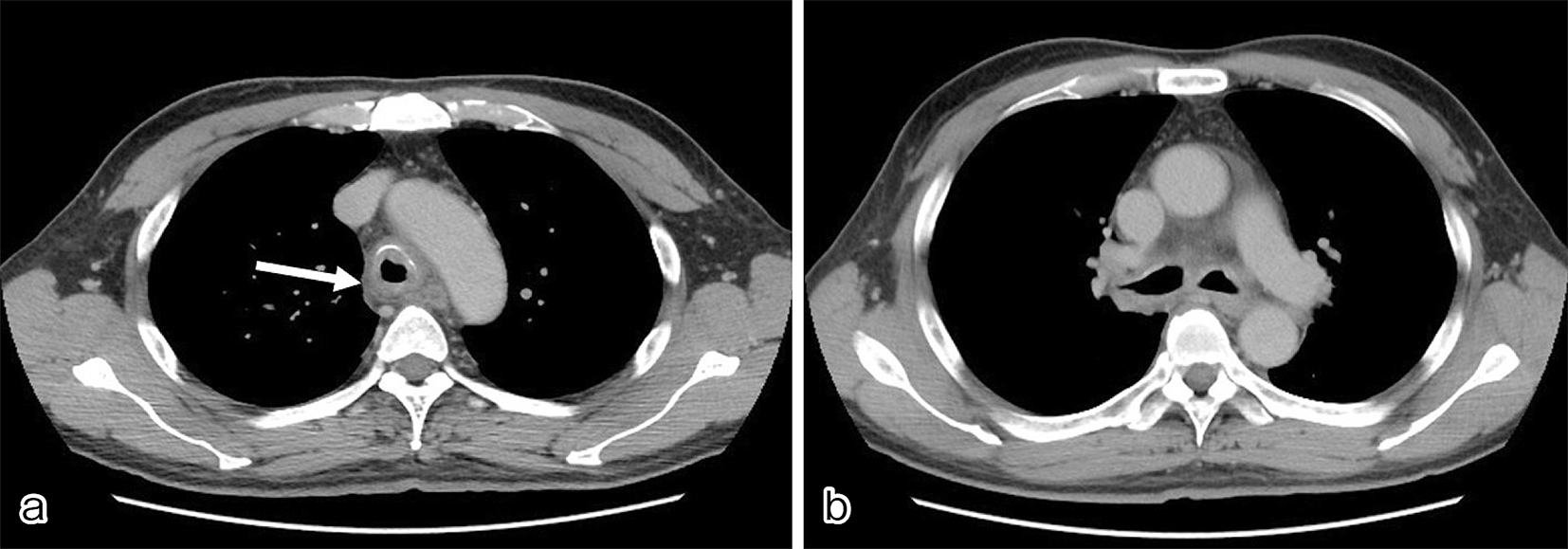
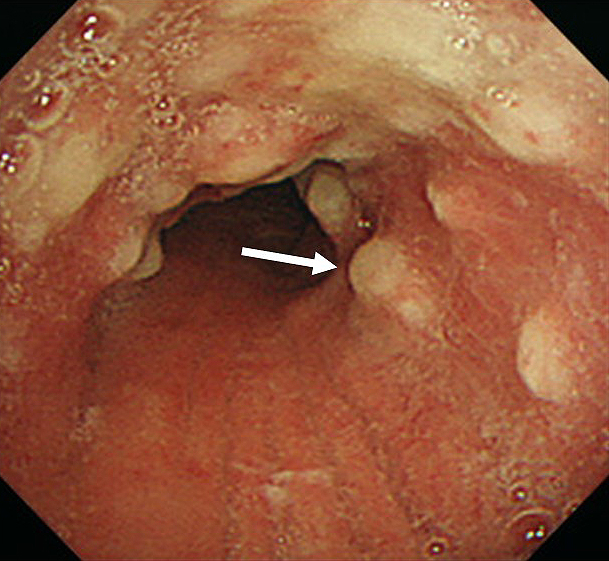
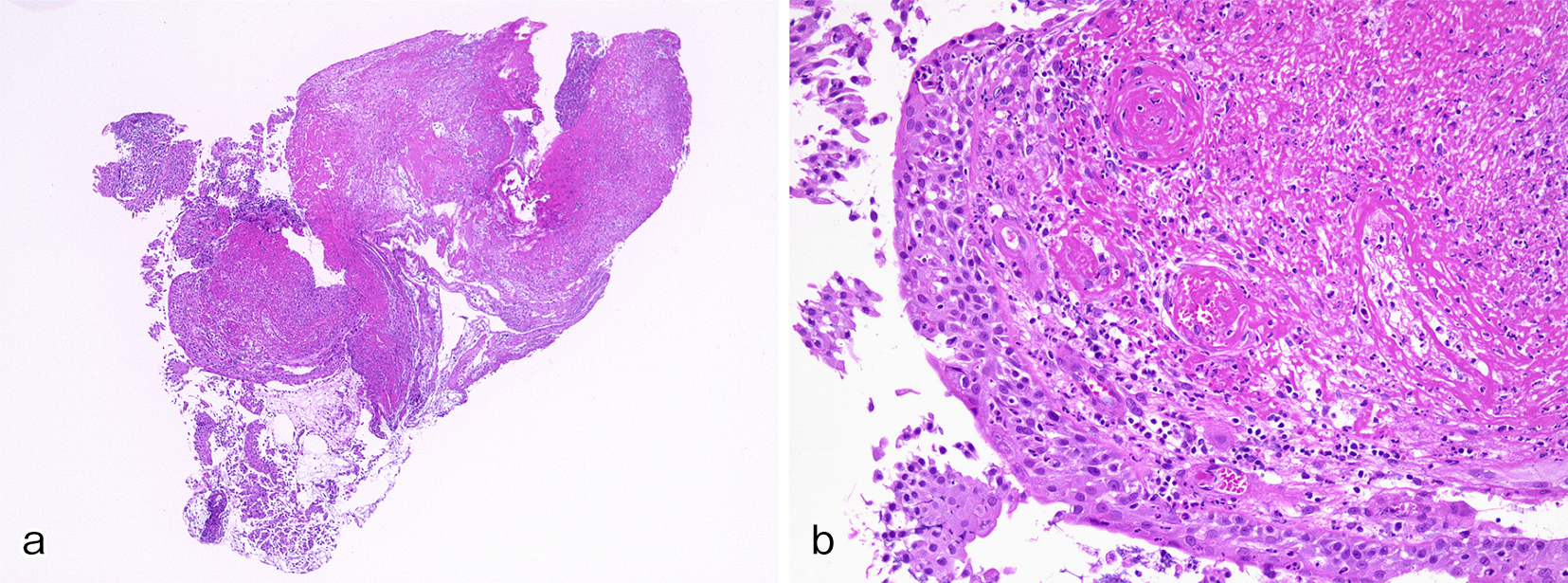
A 61-year-old man with a history of sinusitis was admitted due to fever, pain in the left side of the nose, and arthralgia. Clinical examination showed tenderness and swelling of the left nasal cartilage, left knee joint, and left sternoclavicular joint. Contrast-enhanced computed tomography (CT) was performed on the next day because he developed cough and dyspnea. CT revealed thickening of the tracheal and bilateral bronchial tube walls (Figure 1a, b); bronchoscopy showed remarkable redness of the bronchial mucosa, and white lesions were observed except in the membranous portion (Figure 2). Tracheal biopsy revealed acute inflammation (Figure 3a, b). Relapsing polychondritis (RP) was diagnosed, and prednisolone (1 mg/kg; 60 mg/body) was administered. Consequently, his symptoms were resolved, and the laryngo-tracheobronchial luminal narrowing and wall thickening improved. RP is an autoimmune disease characterized by inflammation and destruction of cartilaginous tissues and can affect several organs. RP complicated by laryngo-tracheobronchial disease may lead to airway obstruction, resulting in even death (1).
None
Daisuke Taniyama, Taketomo Maruki, and Tetsuya Sakai contributed to the report concept and design.
Daisuke Taniyama and Tetsuya Sakai performed the acquisition of patient’s data.
Daisuke Taniyama prepared and wrote the manuscript.
Informed consent has been obtained from the patient to publish the information, including their photographs.
In this study, IRB approval was not required.
Emmungil H, Aydin SZ. Relapsing Polychondritis. Eur J Rheumatol. 2015;2(4):155-9.