Corresponding author: Ana Lilia Peralta-Amaro, ranitaper22@hotmail.com
DOI: 10.31662/jmaj.2022-0194
Received: October 26, 2022
Accepted: January 16, 2023
Advance Publication: March 24, 2023
Published: April 14, 2023
Cite this article as:
Peralta-Amaro AL, Márquez-Vargas MG, González-Molinero JC, Cruz-Gómez MdJ, Gómez-Piña JJ, Hernández-Jiménez CA, Cabrera-Castillo TS, Lucas-Hernández A, Carus-Sánchez A, Alvarado-García MA, Cruz-González L. Type D Adipsia with Severe Hypernatremia: A Unique Presentation of an Extensive Intracranial Germinoma. JMA J. 2023;6(2):226-229.
Intracranial germ cell tumors are uncommon brain tumors; germinoma is the most common tumor in children and young adults, and the most common regions affected are pineal gland and suprasellar region. Germinomas of the suprasellar region are accompanied by endocrine alterations, with adipsia being a rare presentation. Here, we present the case of a patient with an extensive intracranial germinoma whose initial presentation was adipsia, without any other endocrinological alteration, with development of severe hypernatremia and unusual manifestations derived from it, such as deep vein thrombosis, myopathy with rhabdomyolysis, and neurological axonal damage.
Key words: intracranial germinoma, hypernatremia, adipsia
Intracranial germ cell tumors (icGs) are rare neoplasms that represent between 0.5% and 2.1% of primary brain tumors in children and adolescents; two-thirds are germinomas, and the rest are nongerminomas. Clinical manifestations of icGs depend on the location and size of the tumor. In addition, icGs are considered highly curable brain tumors (1).
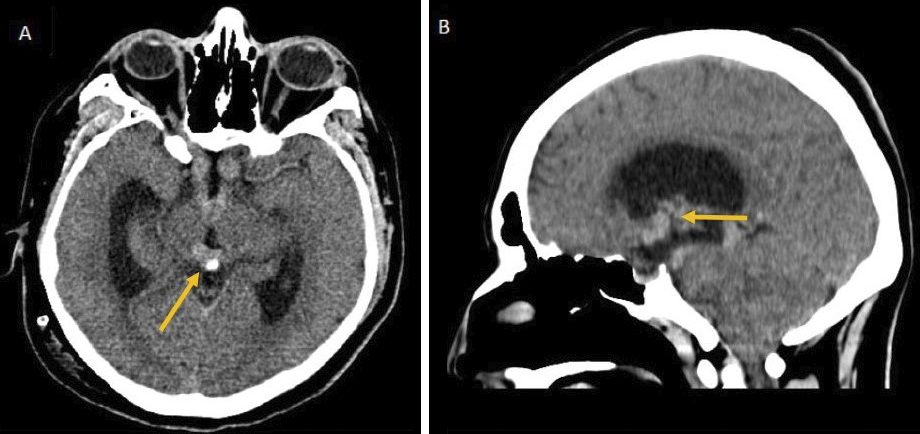
A 22-year-old man came to our hospital due to a six-month-long generalized decrease in muscle strength. Regarding important background, nine months ago he presented with decreased visual acuity of the right eye and then hydrocephalus with intracranial hypertension, for which a ventriculoperitoneal bypass valve was placed. Next, brain computed tomography (CT) showed a lobulated hyperdense tumor with different locations: suprasellar, infundibular, and pineal, with hydrocephalus (Figure 1). Three months later, he presented with thrombosis of the iliac vein and left common femoral vein, and he received rivaroxaban 20 mg q24h, without any medical follow-up.
On physical examination, we found a pale patient with dehydrated oral mucosa, and the neurological examination showed the following: visual acuity of the right eye 20/200 and the left 20/100, no papilledema, bitemporal hemianopsia, and Parinaud’s syndrome (downward conjugate gaze in primary position with bilateral limited supraversion, dilated pupils with hyporeflexia, and upgaze convergence nystagmus). Moreover, he presented with decreased muscle tone and strength (4/5 thoracic limbs and 3/5 pelvic limbs), decreased tendon reflexes, and ataxic gait.
Further, his laboratory tests showed anemia, elevated lactate dehydrogenase, hypernatremia, and elevated creatine phosphokinase. During his hospitalization, hypernatremia was confirmed (sodium 170-182 mEq/L) with a serum osmolarity of 353.4 mOsm/kg. Urinary osmolarity and urinary specific gravity were normal (Table 1). Further, in the laboratory tests of nine months ago, the hypernatremia also stood out (sodium 185 mEq/L).
Table 1. Laboratory Tests.
| Value | Reference Value | |
|---|---|---|
| Blood chemistry | ||
| Glucose, mg/dL | 103.1 | 70-105 |
| Creatinine, mg/dL | 1.26 | 0.5-0.9 |
| Albumin, mg/dL | 4.1 | 3.4-5 |
| Alanine aminotransferase, UI/L | 25.6 | 13-40 |
| Total Bilirubin, mg/dL | 0.42 | 0.2-1 |
| Lactate dehydrogenase, UI/L | 463 | 180-250 |
| Serum electrolytes | ||
| Sodium, mEq/L | 172 | 136-145 |
| Potassium, mEq/L | 4.3 | 3.5-5 |
| Creatinine phosphokinase, UI/L | 11,236 | 24-195 |
| Complete Blood Count | ||
| Hemoglobin, g/dL | 10.2 | 12-18 |
| Hematocrit, % | 36.1 | 37-52 |
| Leukocyte, K/μL | 9.5 | 4.5-10 |
| Neutrophils, K/μL | 8.3 | 3.0-6.9 |
| Lymphocyte, K/μL | 0.8 | 0.6-3.4 |
| Platelets, K/μL | 144 | 150-400 |
| Prothrombin time, s | 15 | 11-15 |
| Partial thromboplastin time, s | 33 | 30-40 |
| General urine test | ||
| Color | Light yellow | Light |
| Density | 1.010 | 1.005-1.030 |
| Nitrites | Negative | Negative |
| Glucose | Negative | Negative |
| Tumor markers | ||
| Carcinoembryonic antigen, ng/mL | 0.38 | 0-2.5 |
| Alpha-fetoprotein, ng/mL | 2.93 | < 40 |
| Carbohydrate antigen 19.9, UI/mL | 5.1 | < 30 |
| Hormone test | ||
| Total Triiodothyronine T3, ng/dL | 121.17 | 64-181 |
| Thyroxine T4, ng/dL | 0.57 | 0.53-1.34 |
| Thyroid stimulating hormone, μUI/mL | 2.38 | 0.4-4.94 |
| Prolactin, ng/mL | 16.59 | 2.5-17 |
| Adrenocorticotropic hormone, pg/mL | 42.82 | 0-46 |
| Cortisol, μg/dL | 8.24 | 5-25 |
| Growth hormone, ng/mL | 0.12 | 0.05-1 |
| Osmolality | ||
| Serum osmolality, mOsm/kg | 353.4 | 280-300 |
| Urine osmolality, mOsm/kg | 350 | 50-1200 |
The patient did not manifest thirst and did not present with polyuria. In addition, he was treated with hypotonic solutions with maximal sodium decreasing to 160 mEq/L.
To assess the current characteristics of the lesion observed in the previous brain CT, a brain magnetic resonance imaging with contrast was performed. It showed a hypothalamic-chiasmatic tumor with extension to the pineal gland through the floor of the third ventricle (FTV) (Figure 2). The biopsy of the tumor reported germinoma. Testicular ultrasound showed no evidence of tumor, and the CT scan ruled out metastases. Hormonal function of anterior pituitary and blood levels of β-human chorionic gonadotropin and alpha-fetoprotein were normal (Table 1). Next, electromyography and conduction velocities showed muscle membrane instability and a sensorimotor polyneuropathy with axonal damage.
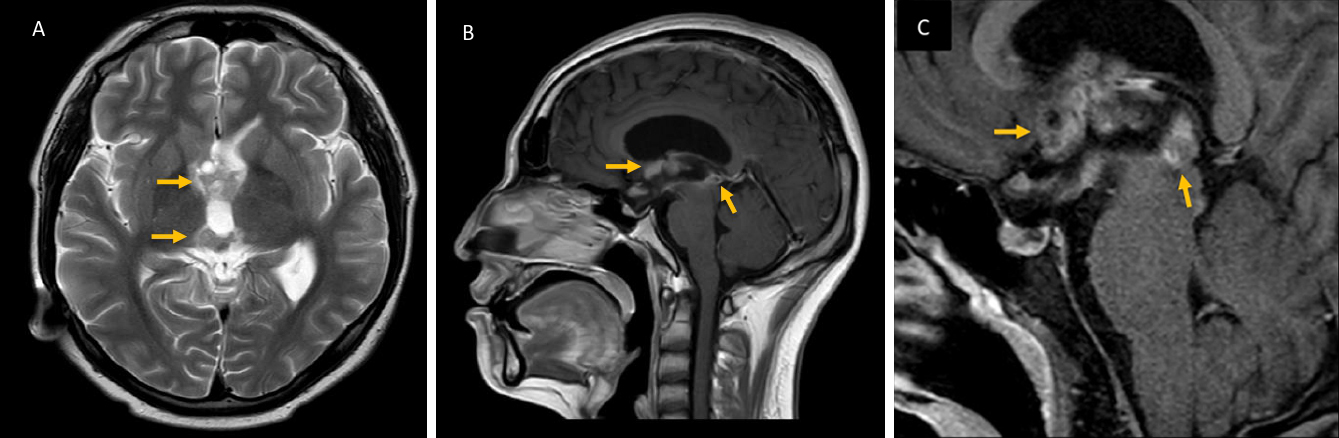
The final diagnosis was adipsia with severe hypernatremia secondary to primary extragonadal germinoma of the hypothalamus with extension to the chiasmatic region and pineal gland through the FTV. The patient received radiotherapy and sequential chemotherapy with ifosfamide and cisplatin, with which he presented with a complete response.
Endocrinological alterations can be part of the presentation of germinomas of suprasellar region (SSR) or present as a complication of treatment. The most frequently reported endocrine disorder is diabetes insipidus (DI), which is characterized by polydipsia and polyuria (urinary volume > 300 ml/hr or >4 liters/day, with urinary osmolarity <200 mOsm/kg and urinary density <1.005) (1), (2), (3).
Adipsia is a rare endocrine disorder which is caused by damage to the circumventricular organs of the anterior hypothalamus where the thirst osmoreceptors are located. Adipsic patients do not perceive osmotic dehydration and therefore do not respond with an adequate increase in fluid intake, leading to the development of hypernatremia. The hypernatremia can be complicated by thrombotic episodes, rhabdomyolysis, and peripheral neurological damage (2). Next, adipsia can be divided into the following four types: Type A adipsia, also known as essential hypernatremia or partial DI, is characterized in that patients are thirsty and secrete vasopressin, which allows them to be protected from severe hypernatremia. Type B adipsia, is where patients demonstrate a normal osmoregulatory set point, but thirst and vasopressin responses to a hyperosmolar challenge are insufficient to preserve this set point. Type C adipsia, is where a widespread central destruction occurs leading to a complete absence of vasopressin release and thirst response in the presence of an osmotic stimulus, and such a combination is termed adipsic DI (ADI). Currently, three cases of icG with ADI as part of their presentation exist, one of them bifocal (3), (4), (5). Lastly, Type D adipsia, an extremely rare condition, is where the osmoregulation of vasopressin release is intact, but the thirst response is absent (2).
Like Alhassan MA, et al. (6), we considered that our patient demonstrated the integrity of the vasopressin osmoregulation, since he presented with normal urinary osmolarity. In addition, DI was ruled out due to the absence of polyuria, including masked DI, since polyuria did not occur after intravenous hydration and no other signs of hypocortisolism were found. Therefore, the possibility exists that our patient’s adipsia was Type D, although in our setting, performing osmoregulation tests was not possible, as in other reported cases of Type D adipsia (7).
Finally, no other case was found in the literature in which adipsia was the only endocrine disorder in the initial presentation of an intracranial germinoma.
None
All authors participated in the acquisition and interpretation of data, as well as in the writing, revision, and final approval of the manuscript. All authors meet the ICMJE authorship criteria.
Consent to publish was obtained from the patient.
Jorsal T, Rørth M. Intracranial germ cell tumours. A review with special reference to endocrine manifestations. Acta Oncol. 2012;51(1):3-9.
Cuesta M, Hannon MJ, Thompson CJ. Adipsic diabetes insipidus in adult patients. Pituitary. 2017;20(3):372-80.
Arai K, Akimoto H, Inokami T, et al. Marked hypernatremia in suprasellar germinoma lacking a sense of thirst. Nihon. Jinzo Gakkai Shi. 1999;41(8):804-12. Japanese.
Kreutz J, Potorac I, Lutteri L, et al. Adipsic diabetes insipidus revealing a bifocal intracranial germinoma. Ann Endocrinol. 2017;78(3):141-5.
Căpraru OM, Paşcanu I, Mărginean OC. Suprasellar germinoma with chronic hypernatremia, adipsic diabetes insipidus and hypopituitarism. Case report. Acta Endocrinol. 2014;10(2):273-82.
Alhassan MA, Abdalla AT, Hassan SS, et al. Adipsic hypernatremia in a young Sudanese child, challenges in a limited-resource setting: a case report. Pan Afr Med J. 2021;38:86.
Chothia MY, George K, Sheik M, et al. Hypodipsic-hypernatremia syndrome in an adult with polycythemia: a case report. J Med Case Rep. 2018;12(1):381.