Corresponding author: Ryoukichi Ikeda, ryoukich@hotmail.com
DOI: 10.31662/jmaj.2020-0007
Received: February 5, 2020
Accepted: February 25, 2020
Advance Publication: April 6, 2020
Published: April 15, 2020
Cite this article as:
Ikeda R, Kikuchi T, Oshima H, Kobayashi T. Management of Patulous Eustachian Tube. JMA J. 2020;3(2):101-108.
Patients with patulous Eustachian tubes (PET) suffer from annoying aural symptoms, such as voice or breath autophony, and aural fullness due to the ET’s abnormal patency. It may lead to an enormous reduction in quality of life. Various treatment methods, including conservative and surgical therapy, have been reported. In most cases, conservative treatment is sufficient to relieve patients of aural symptoms. However, some chronic and severe cases are resistant to traditional conservative therapy. Recently performed prospective and multicenter trials revealed the efficacy and safety of a silicone plug (Kobayashi plug) insertion for patients with severe PET. Patulous Eustachian tube handicap inventory-10 (PHI-10), tubal obstruction procedures, sitting computed tomography (CT), and ET function tests (tubo-tympano-aerodynamic graphy (TTAG) and sonotubometry) are useful for diagnosis as well as selecting candidates for surgery in severe cases.
Key words: Eustachian tube, patulous Eustachian tube, surgical treatment, tympanic membrane, silicone plug
The Eustachian tube (ET) is the connection between the middle ear and nasopharyngeal space. It is closed under normal conditions and opens temporarily during swallowing (1), (2). The closed ET protects the middle ear from unwanted acoustic energy transmission from the nasopharynx, which is generated by self-vocalization and breathing. Patients with patulous ET (PET) suffer from annoying aural symptoms, such as aural fullness, voice, or breath autophony, due to the ET’s abnormal patency (3), reducing quality of life enormously. Various treatment methods have been reported (4), (5) but some controversy remains. In this review, we will describe treatments for this challenging disease.
In most cases, PET symptoms can be alleviated by patient explanation. This entails explaining the disease and mechanisms leading to symptom manifestation to the patient, providing reassurance, offering specific lifestyle guidance (rehydrating sufficiently during summer or after vigorous activity, avoiding weight loss, etc.), and prescribing conservative therapy (4). Self-instillation of physiological saline solution has been reported to be effective in controlling PET symptoms (6). Mucous-thickening agents (7) and topical irritants (e.g., Lugol-gel (8), (9), Bezold powder, or sodium iodide) to induce mucosal edema of the pharyngeal orifice can also provide temporary symptom relief.
Applying a paper patch to the tympanic membrane (TM) has also been proposed (10). A piece of steri strip (3M, Maplewood, USA), cut into a circular shape about 5 mm in diameter, was placed on the posterior-superior quadrant of the TM. It was reported to be effective in some PET cases where the primary symptom was aural fullness.
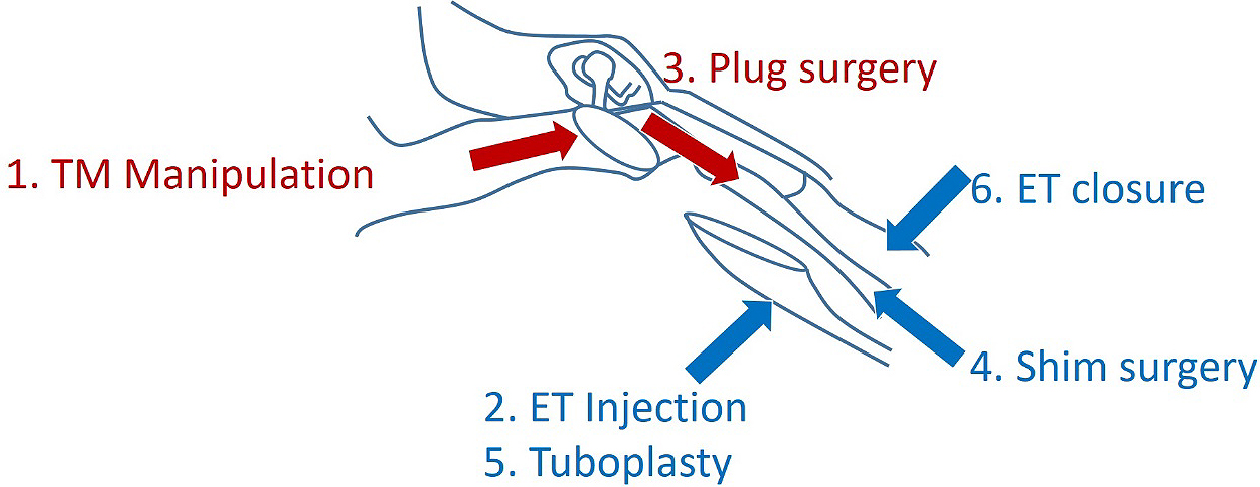
For chronic and severe cases resistant to conservative therapy, surgical procedures are considered. Surgical procedures are categorized by the procedure type, including TM manipulation (tympanostomy tube insertion and mass loading of the TM), plug surgery, ET injection, shim surgery, tuboplasty, and ET closure (4), (5). The former two methods are usually performed via a transtympanic approach, and the latter three treatments via a transnasal approach (Figure 1). A recent systematic review of PET surgical treatment revealed that plug surgery and shim surgery had shown relatively high efficacy and safety (unpublished data). The transtympanic silicone plug (Kobayashi Plug) insertion is categorized under plug surgery and is used for severe PET cases in Japan.
Bluestone et al. first described plugging the ET through the middle ear (11). They used an intravenous indwelling catheter; its lumen was filled with methyl methacrylate. The anterior tympanomeatal flap was raised, and a tympanostomy tube insertion was performed at the same time as plugging. We have developed a specially designed silicone plug (Kobayashi Plug) for treating patients with severe (9), (12), (13), (14), (15). The early prototype plug is smaller than the currently used type (Figure 2). The current type has a length of 23 mm and comes in different plug sizes, with differing tip diameters, to accommodate the ET variation in PET cases (type 3; 1.5mm to 9; 4.0mm) (Figure 3). The plug is slightly bent at the tip to facilitate insertion into the ET. A wing-like protrusion was designed for each tail of the plug to prevent descent into the nasopharynx, a problem frequently experienced by patients using the prototype plug, which lacked wing-like protrusions (13). This surgery is usually performed in cases of intractable “Definite PET” diagnosed by the JOS Diagnostic Criteria (16), (17) (Table 1) and resistant to at least six months of various conservative treatment methods (18). We have completed a prospective multicenter clinical trial in Japan supported by the development of New Drugs and Medical Devices (Japan Medical Association) from the Japan Agency for Medical Research and development, AMED.

Table 1. The Japan Otological Society Diagnostic Criteria for PET.
| 1. There are subjective symptoms |
| One or more of the following symptoms included: voice or breath autophony, and aural fullness |
| 2. Tubal obstruction procedures (A or B) clearly improves symptoms |
| A. Posture change to the supine / lordotic positon |
| B. Pharyngeal orifice obstruction procedure (swab, gel, etc.) |
| 3. There is at least one of the following objective findings of patent E-tube: |
| A. Respiratory fluctuation of the tympanic membrane |
| B. Variations of external auditory canal pressure synchronized with nasopharyngeal pressure |
| C. The sonotubometry shows (1) the probe tone sound pressure level is less than 100 dB or (2) an open plateau pattern. |
| Definite Patulous Eustachian tube (PET): 1 + 2 + 3 |
| Possible Patulous Eustachian tube (PET) : 1+ (2 or 3) |
We previously reported 252 ears of 191 patients with PET who received a Kobayashi Plug insertion (13). The overall success rate was 83.0%. Furthermore, a prospective, multicenter trial was conducted for 30 patients with PET. The efficacy and safety of 28 and 27 patients, respectively, were analyzed. Twenty-three cases (82.1%) were considered successful (18).
No severe or life-threatening complications have been observed. In a prospective, multicenter clinical trial (29 cases) (18), middle ear effusions (MEE), including transient effusions, occurred in 17.2% of cases. One case (3.4%) received a ventilation tube insertion for persistent MEE. TM perforation was found in 13.8%. No plug descent to the nasopharynx occurred. The hearing threshold (the pure-tone average of 0.5, 1, and 2 kHz of air-conduction) at the time of screening was 16.3±9 and at 3 and 6 months post-operatively were 18.6±10.9 dB HL and 18.6±13 dB HL, respectively, with no significant difference.
Subjective findings
Subjective symptoms are evaluated by the patulous Eustachian tube handicap inventory-10 (PHI-10)(19) (Table 2). The classification for grading severity is defined as 1) no handicap (0–8), 2) mild handicap (10–16), 3) moderate handicap (18–24), and 4) severe handicap (26–40). With respect to evaluation after surgery, no handicap (0–8) and mild handicap (10-16) are considered successful outcomes.
Table 2. Patulous Eustachian Tube Handicap Inventory-10 (PHI-10). 1) No Handicap (0–8). 2) Mild Handicap (10–16). 3) Moderate Handicap (18–24). 4) Severe Handicap (26–40).
| No | Question | yes: 4 | sometimes: 2 | no: 0 |
|---|---|---|---|---|
| 1 | Because of your symptom is it difficult for you to concentrate? | |||
| 2 | Does the loudness of your symptom make it difficult for you to hear people? | |||
| 3 | Does your symptom make you angry? | |||
| 4 | Do you fell as though you cannot escape your symptom? | |||
| 5 | Does your symptom interfere with your ability to enjoy social activities? | |||
| 6 | Because of your symptom do you feel frustrated? | |||
| 7 | Does your symptom interfere with your job or household responsibilities? | |||
| 8 | Do you feel that your symptom has placed stress on your relationships with members of your family and friends? | |||
| 9 | Do you find it difficult to focus your attention away from your symptom and on to other things? | |||
| 10 | Does your symptom make you feel anxious? |
Tubal obstruction procedures
Before assessing improvement of symptoms after surgery, it should first be ascertained that the patient does indeed have “definite PET” by obstructing the ET's pharyngeal orifice. This occlusion is done transnasally using a swab, gel, etc., preoperatively (Figure 4), and if the patient’s aural symptoms do not improve after this maneuver, their symptoms are not due to PET. They may be due to other diseases, such as superior canal dehiscence syndrome sensorineural hearing loss, etc.
Sitting CT findings
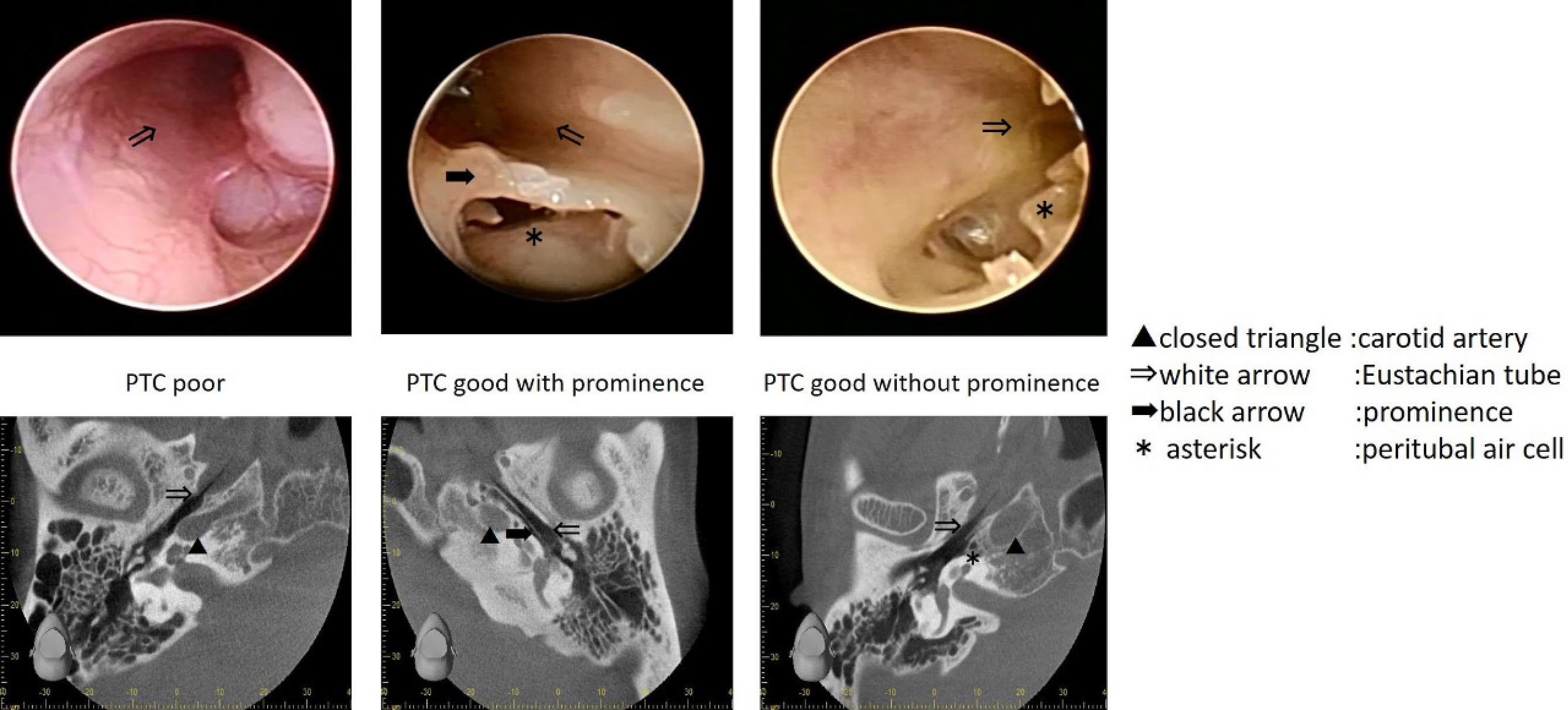
Sitting computed tomography (CT) is essential for preoperative ET evaluation by delineating the ET lumen’s shape throughout its course from the nasopharynx to the tympanic orifice (20), (21), (22), (23), (24). The anatomy of the ET’s tympanic portion is variable and categorized into three types, namely poor peritubal cell (PTC) types (Figure 5: left), good PTC types with prominence (Figure 5: middle), and good PTC types without prominence (Figure 5: right) (25). The good PTC type with prominence (Figure 5: middle) has a significantly smaller tympanic orifice width than the other types. The good PTC type, with prominence, has a false passage due to the ridge of bony prominence separating the ET’s tympanic portion into a lateral opening for the ET (26). Therefore, plug surgery is can be more difficult in this type than in the two other types.
ET function test
ET function tests, such as tubo-tympano-aerodynamic graphy (TTAG) (27) and sonotubometry (28), were performed using a commercially available machine (JK05AD; Rion, Tokyo, Japan). Pressure changes in the external auditory canal (EAC) and the nasopharynx were coincidentally recorded using the TTAG’s manometry mode. Positive TTAG findings were determined as an EAC pressure change synchronous with that in the ipsilateral nasopharynx (Figure 6: upper). Sonotubometry automatically creates the input sound pressure level (SPL) at the nostril that enables a pre-set level of 50 dB SPL output in the EAC. Two findings were considered consistent with a patent ET, i.e. lowering of probe tone SPL to below 100 dB (Figure 6: lower left) or an “open plateau pattern” when the ET opens upon swallowing and remains open (Figure 6: lower right).
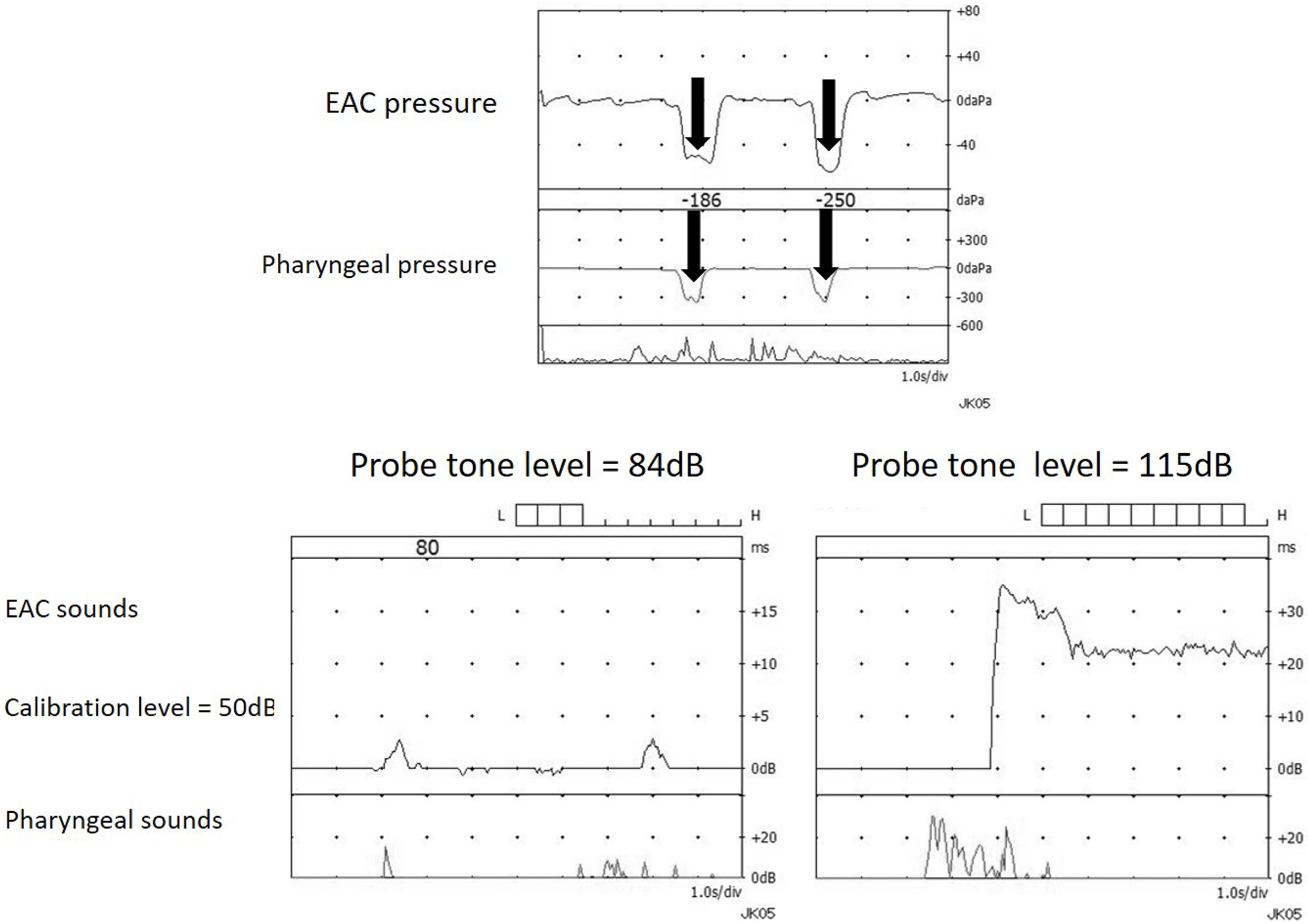
Sound transmission assessed by sonotubometry is more useful than pressure transmission assessed by TTAG in predicting PET’s morphological severity (29), (30). Thus, the sitting CT and sonotubometry are valuable tools to aid in plug size selection. Based on our previous study (31), we recommend the initial Kobayashi Plug size selection, based on preoperative probe tone SPL, using sonotubometry as follows: size #4; over 95dB, size #5; between 94 and 85 dB, size #6; lower than 84dB.
This surgery can be performed at either the outpatient clinic or in an operating room. We usually conducted this procedure in an operating room.
1. After draping, the EAC is anesthetized with an injection of 0.5–1.0 mL of 1% lidocaine at the EAC.
2. A small myringotomy (3 mm long) is performed in the TM’s anterosuperior quadrant (Figure 7-1).
3. The ET’s tympanic portion can be visualized directly via a myringotomy hole by 30-degree endoscopy with a 2.7mm diameter (Figure 7-2).
4. Local anesthesia (step 1) is not sufficient for analgesia in the ET’s bony and cartilage portion, so 0.05 ml of 4% lidocaine solution is sprayed onto the bony portion of the ET directly (Figure 7-3). Patients are advised to position themselves with the affected ear pointing straight up toward the ceiling. The posterior tympanic cavity is filled with a saline solution before spraying lidocaine to prevent vertigo due to inner ear anesthesia.
4. The plug body is made such that it is bent slightly toward the tip to facilitate insertion from a small myringotomy hole (Figure 7-4). After the tip is inserted, the plug is laid down toward the TM and inserted gently, sliding on the TM surface (Figure 7-5 and 6). If resistance is felt during insertion, the plug status should be checked via endoscopy. When a plug does not advance, in spite of being inserted into the ET, changing the plug to a smaller size should be considered. Adequate plug size is determined when slight resistance is felt. If no resistance is felt, the plug size may be too small.
5. The plug position is checked with 30-degree endoscopy inserted medial to the TM (Figure 7-7).
6. The middle ear is rinsed with 10 ml of the saline solution after inserting the plug.
7. A piece of paper is applied to patch the myringotomy hole (Figure 7-8).
This review identifies and summarizes the existing evidence for conservative and surgical treatment of PET symptoms. Plug surgery, especially Kobayashi plug surgery, is effective and safe for severe PET cases. Moreover, multifaceted evaluation of the ET condition is essential to manage patients with PET.
This article is based on the study, which received the Medical Research Encouragement Prize of The Japan Medical Association in 2019.
None
This work was supported by JSPS KAKENHI grant number 15K20175, 18K16872 and the Project Promoting Clinical Trials for Development of New Drugs and Medical Devices (Japan Medical Association) from Japan Agency for Medical Research and development, AMED grant number CCT-B-2806.
Bluestone CD, Hebda PA, Alper CM, et al. Recent advances in otitis media. 2. Eustachian tube, middle ear, and mastoid anatomy; physiology, pathophysiology, and pathogenesis. Ann Otol Rhinol Laryngol Suppl. 2005;194:16-30.
Sudhoff HH, Mueller S. Treatment of pharyngotympanic tube dysfunction. Auris Nasus Larynx. 2018;45(2):207-14.
Hori Y, Kawase T, Oshima T, et al. Objective assessment of autophony in patients with patulous Eustachian tube. Eur Arch Otorhinolaryngol. 2007;264(12):1387-91.
Luu K, Remillard A, Fandino M, et al. Treatment effectiveness for symptoms of patulous eustachian tube: A systematic review. Otol Neurotol. 2015;36(10):1593-600.
Hussein AA, Adams AS, Turner JH. Surgical management of Patulous eustachian tube: A systematic review. Laryngoscope. 2015;125(9):2193-8.
Oshima T, Kikuchi T, Kawase T, et al. Nasal instillation of physiological saline for patulous eustachian tube. Acta Otolaryngol. 2010;130(5):550-3.
Ohta S, Sakagami M, Suzuki M, et al. Eustachian tube function and habitual sniffing in middle ear cholesteatoma. Otol Neurotol. 2009;30(1):48-53.
Kawase T, Hori Y, Kikuchi T, et al. Patulous Eustachian tube associated with hemodialysis. Eur Arch Otorhinolaryngol. 2007;264(6):601-5.
Ikeda R, Oshima T, Oshima H, et al. Management of patulous eustachian tube with habitual sniffing. Otol Neurotol. 2011;32(5):790-3.
Murakami S, Nakazawa M, Watanabe N, et al. Role of tympanic membrane in symptoms of patulous Eustachian tube syndrome; A new treatment with use of adhesive tape on the tympanic membrane. Middle Ear Mechanics in Research and Otology Proc 3rd Symp. 2004:438-40.
Bluestone CD, Cantekin EI. "How I do it"--otology and neurotology. A specific issue and its solution. Management of the patulous Eustachian tube. Laryngoscope. 1981;91(1):149-52.
Sato T, Kawase T, Yano H, et al. Trans-tympanic silicone plug insertion for chronic patulous Eustachian tube. Acta Otolaryngol. 2005;125(11):1158-63.
Kikuchi T, Ikeda R, Oshima H, et al. Effectiveness of Kobayashi plug for 252 ears with chronic patulous Eustachian tube. Acta Otolaryngol. 2017;137(3):253-8.
Ikeda R, Kikuchi T, Kobayashi T. Endoscope-assisted silicone plug insertion for patulous Eustachian tube patients. Laryngoscope. 2017;127(9):2149-51.
Endo S, Mizuta K, Takahashi G, et al. The effect of ventilation tube insertion or trans-tympanic silicone plug insertion on a patulous Eustachian tube. Acta Otolaryngol. 2016;136(6):551-5.
Kobayashi T, Morita M, Yoshioka S, et al. Diagnostic criteria for Patulous Eustachian Tube: A proposal by the Japan Otological Society. Auris Nasus Larynx. 2018;45(1):1-5.
Kawamura Y, Ikeda R, Kikuchi T, et al. The characteristic of patulous eustachian tube patients diagnosed by the JOS diagnostic criteria. PLoS One. 2019;14(12):e0226908.
Ikeda R, Oshima T, Mizuta K, et al. Efficacy of a silicone plug for patulous eustachian tube: A prospective, multicenter case series. Laryngoscope. 2019.
Ikeda R, Kikuchi T, Oshima H, et al. New scoring system for evaluating Patulous Eustachian tube patients. Otol Neurotol. 2017;38(5):708-13.
Yoshida H, Kobayashi T, Morikawa M, et al. CT imaging of the patulous eustachian tube--comparison between sitting and recumbent positions. Auris Nasus Larynx. 2003;30(2):135-40.
Yoshida H, Kobayashi T, Takasaki K, et al. Imaging of the patulous Eustachian tube: high-resolution CT evaluation with multiplanar reconstruction technique. Acta Otolaryngol. 2004;124(8):918-23.
Kikuchi T, Oshima T, Ogura M, et al. Three-dimensional computed tomography imaging in the sitting position for the diagnosis of patulous eustachian tube. Otol Neurotol. 2007;28(2):199-203.
Kikuchi T, Oshima T, Hori Y, et al. Three-dimensional computed tomography imaging of the eustachian tube lumen in patients with patulous eustachian tube. ORL J Otorhinolaryngol Relat Spec. 2009;71(6):312-6.
Ikeda R, Kikuchi T, Oshima H, et al. Relationship between clinical test results and morphologic severity demonstrated by sitting 3-D CT in patients with Patulous Eustachian tube. Otol Neurotol. 2016;37(7):908-13.
Ikeda R, Kikuchi T, Oshima H, et al. Computed tomography findings of the bony portion of the Eustachian tube with or without patulous Eustachian tube patients. Eur Arch Otorhinolaryngol. 2017;274(2):781-6.
Tarabichi M, Najmi M. Transtympanic dilatation of the eustachian tube during chronic ear surgery. Acta Otolaryngol. 2015;135(7):640-4.
Kumazawa T, Honda K, Iwano T, et al. New findings in observations by tubo-tympano-aerodynamic method. Acta Otolaryngol Suppl. 1990;471:25-32.
Perlman H. The eustachian tube: Abnormal patency and normal physiologic state. Arch Otolaryngol. 1939;30:212-38.
Takata I, Ikeda R, Kawase T, et al. Sonotubometric assessment for severity of Patulous Eustachian tube. Otol Neurotol. 2017;38(6):846-52.
Ikeda R, Kawase T, Takata I, et al. Width of Patulous Eustachian tube: Comparison of assessment by sonotubometry and tubo-tympano-aerography. Otol Neurotol. 2019;40(4):e386-92.
Ikeda R, Kikuchi T, Kawamura Y, et al. Plug size selection protocol for the treatment of intractable patulous Eustachian tube with Kobayashi Plug. Acta Oto-Laryngologica. 2019:1-5.